Image caption: Doctors and nurses confer in the Intensive Care Unit of MedStar St. Mary’s Hospital April 8, 2020 in Leonardtown, Maryland. In Maryland, hospital bed capacity is lower than in other states, but has relatively higher physician supply. (Photo by Win McNamee/Getty Images)
Urban areas in California, New York, Louisiana, and Washington State experienced the earliest surges in COVID-19 cases and deaths, but these states are no longer alone — every state has active cases and the numbers keep climbing. Several factors contributed to the spread of the virus nationwide, including higher-than-expected transmission by asymptomatic individuals, early federal missteps in the development and distribution of testing kits, inadequate medical supply distribution, and late and inconsistent social distancing policies. And though the spread and concentration of COVID-19 cases varies across states, most are now scrambling to prepare for worst-case scenarios. Federal agencies and experts are flagging a potential next wave of COVID-19 hotspots across the country.
In this post, we build on our recent analysis by assessing the availability of certain critical health care resources — physician supply, hospital bed capacity, and ventilator supply — as state leaders plan their responses to a potential surge of COVID-19 cases. We also include updated estimates of higher-risk populations based on current guidelines from the Centers for Disease Control and Prevention (CDC). Metrics used for this analysis include:
- share of adult population at higher clinical risk: adults over age 65, and adults ages 18 to 64 with a high-risk chronic illness (i.e., heart disease, chronic obstructive pulmonary disease, asthma, diabetes, or severe obesity)
- physicians per 100,000 residents
- hospital and ICU beds per 1,000 residents, and
- ventilator supply per 100,000 residents.
In Exhibit 1, we take a closer look at the supply of different types of physicians and other health care providers in each state, including the current number of ambulatory and hospital-based physicians, current number of physician assistants and nurse practitioners, and added physician supply under a surge scenario. The states are ordered by the supply of hospital-based physician supply; lighter dots represent higher relative provider supply while the darker dots represent relatively lower supply.
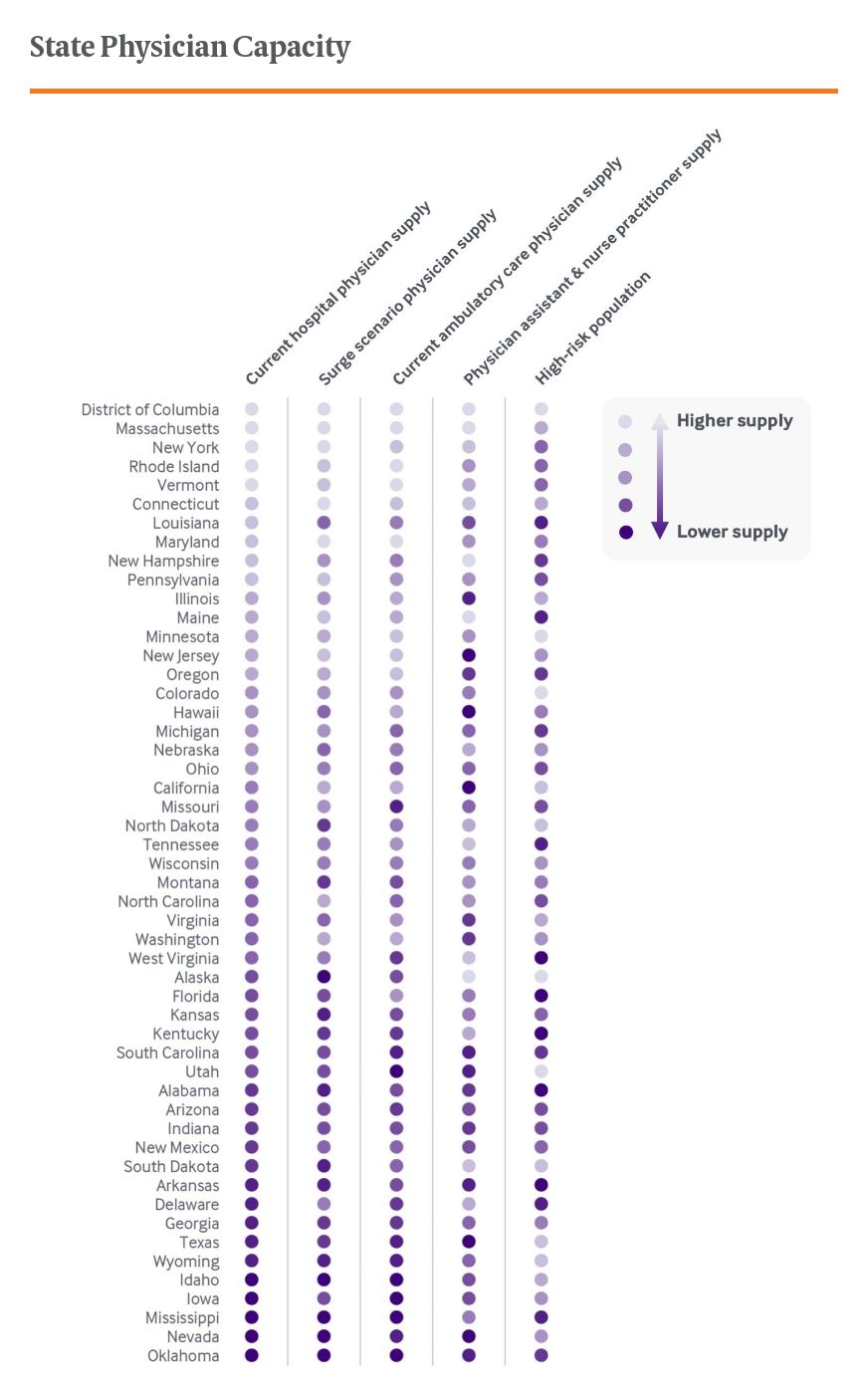
Exhibit 2 is structured similarly but focuses on hospital bed and ventilator supply; states are ordered according to acute hospital bed supply. Both exhibits include an indicator of each state’s high-risk population, including adults age 65 and older and those ages 18 to 64 with a high-risk chronic illness.
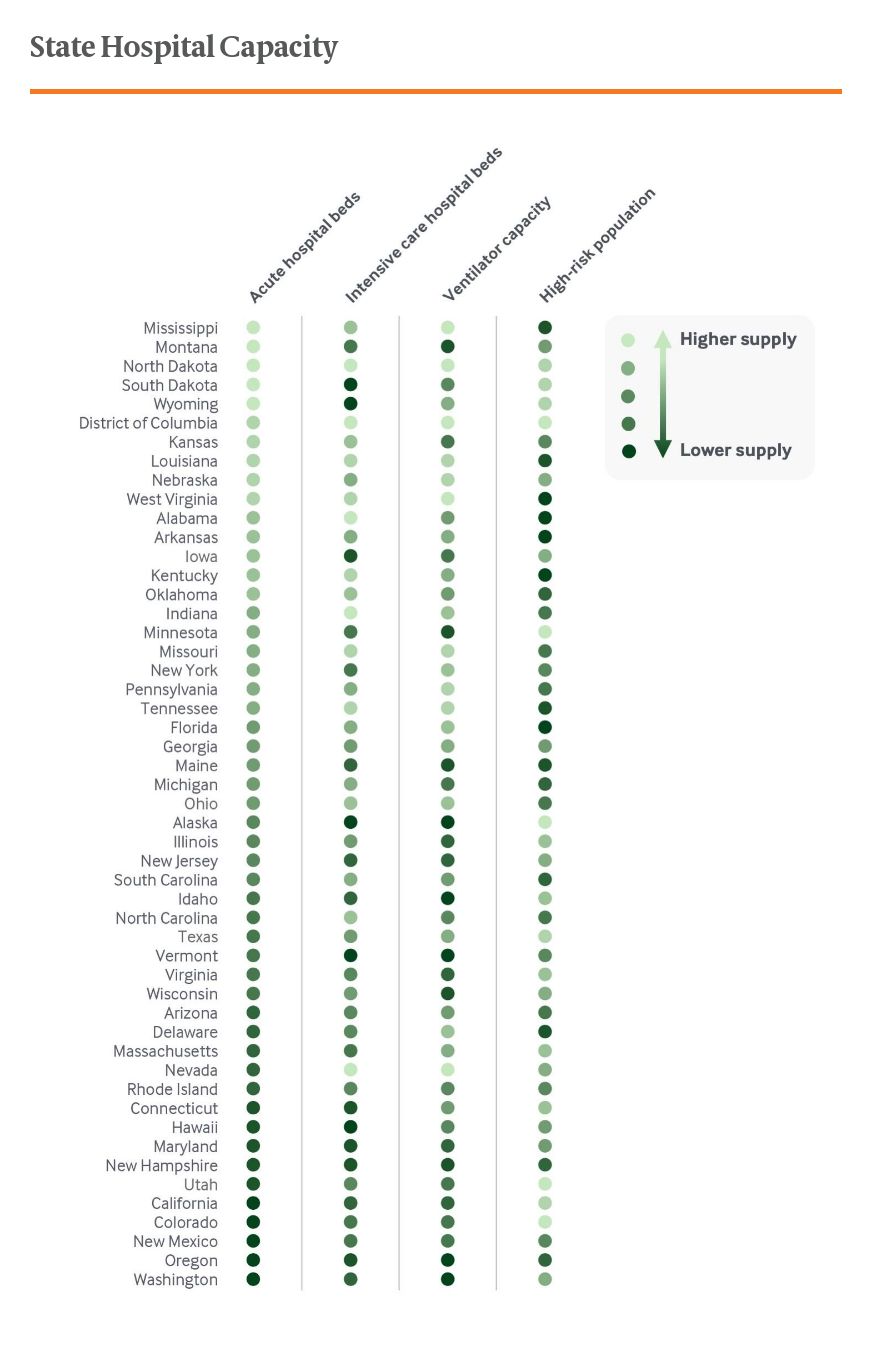
In each of these exhibits, there are several states where the relative provider or hospital capacity tends to cluster either higher or lower than others. This is likely a reflection of variation among health care markets, with capacity shaped by local demand and other factors. But it is also clear that delivery systems in all states would face significant challenges should COVID-19 cases surge in the coming weeks and months. In Maryland, Oregon, and Vermont for example, hospital bed capacity is lower than in other states, but each has relatively higher physician supply. The opposite is true in Arkansas, Indiana, and Kentucky. State health systems also would be forced to confront capacity challenges not measured here, such as nursing shortages.
These analyses cannot forecast the extent to which a COVID-19 surge may or may not overwhelm health care capacity in a given state, but they do provide a snapshot of resource availability and some context for the adjustments that may be needed. As is already becoming apparent in parts of New York, even relatively robust health systems can be overwhelmed quickly by this unprecedented threat. New York also illustrates the level of innovation and flexibility that can be achieved in the face of the threat. Similar surges may hit unprepared states hard, especially where residents have worse access to care.
A global phenomenon, the COVID-19 pandemic is playing out locally. And in the absence of strong federal leadership and chronic federal underinvestment in public health, state governments have emerged as the locus of response. States have several policy levers, ranging from social distancing measures to using the federal waiver process for more flexibility in their Medicaid programs to diverting funds to emergency response. As they do, analysis of variations in state capacity and response can highlight regions and states that may need federal aid and help from others if local outbreaks threaten to overwhelm them.