The COVID-19 pandemic has had a disproportionate effect on Medicare beneficiaries — people age 65 and older, as well as younger beneficiaries with serious disabilities — and has exacerbated existing fault lines within the program. In addition to a higher risk of death or hospitalization, for some beneficiaries COVID-19 has decreased access to in-person care, contributed to declines in mental health, and created additional financial struggles. Congress and the Trump administration responded by waiving or changing current regulations to allow providers flexibility and increased access to care, but many of these changes are temporary. As a result, we do not know their full impact. As more people receive vaccines for COVID-19 and there are fewer virus outbreaks, there may be opportunities to address the existing gaps in Medicare coverage, many of which are highlighted in Commonwealth Fund issue briefs focused on the needs of Medicare beneficiaries during the pandemic.
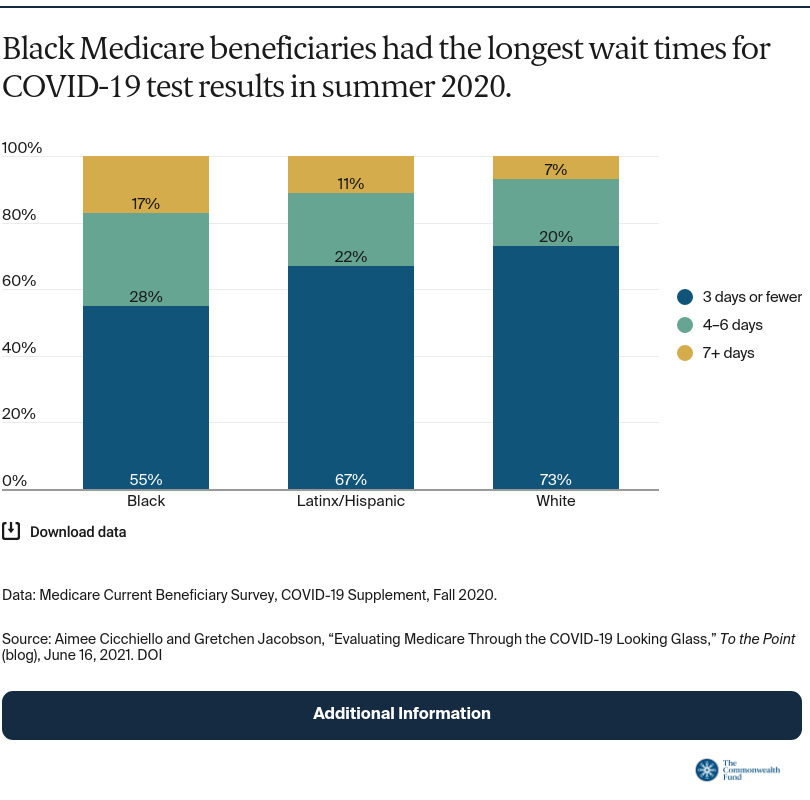
Racial and ethnic disparities. Racial and ethnic disparities among Medicare beneficiaries are well documented; COVID-19 has deepened these divides. Black beneficiaries have been more likely to contract COVID-19 and four times more likely to be hospitalized than white beneficiaries. New data has shown that disparities may extend to accessing COVID-19 care. While rates of COVID-19 testing did not differ by race, wait times for test results had substantial differences early in the pandemic, when testing was often scarce. Nearly three-quarters of white beneficiaries reported waiting three days or fewer in the summer of 2020 to receive results, but only about half of Black beneficiaries received their results in the same time frame. Approximately 17 percent of Black beneficiaries reported waiting a week or more to receive COVID-19 results, compared to 11 percent of Latinx/Hispanic beneficiaries and only 7 percent of white beneficiaries. These disparities may have impeded quarantining and contributed to the spread of the coronavirus in Black and Latinx/Hispanic communities.
Postacute and long-term care. The pandemic has highlighted gaps in coverage and stress points in Medicare’s infrastructure. Nowhere is this more evident than in nursing homes. Cracks in the regulatory framework, little oversight or enforcement, and quality- and infection-control issues contributed to rapidly spreading infections within and between nursing homes. More than a third of COVID-19 deaths have occurred in nursing facilities during the pandemic. Several measures, including reforming Medicare and Medicaid payment rates, increasing enforcement of health and safety standards, and greater investment in nursing workforce could serve to strengthen nursing home quality.
As a consequence of virus outbreaks in nursing homes, more beneficiaries sought out home-based care when it was an option. Home health became important for preventing the spread of COVID-19 and protecting some of the most vulnerable beneficiaries. Yet, home health agencies faced challenges acquiring sufficient supplies of protective equipment and retaining enough trained workers to meet the demand for services. Additionally, there has been relatively little tracking of COVID-19 infections linked to home health care. This is a missed opportunity; creating such a tracking mechanism during the pandemic could have helped to bolster infection control capabilities post-pandemic. As Medicare beneficiaries continue to prefer to receive care in their homes, policy measures that improve the quality of care, strengthen the workforce, and increase the value of the home health benefit will enable Medicare to better meet the needs of beneficiaries.
Access to care. COVID-19 has presented challenges in terms of access to care and could have posed larger issues if the Trump administration had not waived many rules and regulations early on. The administration made more than 200 legislative, regulatory, and subregulatory changes or waivers to Medicare coverage. People with mental health conditions or other chronic conditions have been of particular concern during the pandemic because of social isolation and the need to continually manage their conditions. Telehealth has greatly helped to maintain access to care, and policymakers now face challenges designing optimal Medicare payment and regulatory policies for telehealth in a post-pandemic world. As the Biden administration and Congress deliberate whether to extend telehealth and other policy changes, it is vital to carefully evaluate the potential effects and consequences of making these changes permanent.
Since the first COVID-19 vaccines were administered in December 2020, more than 86 percent of adults age 65 and older have received at least one dose. As more beneficiaries receive immunizations and pandemic precautions are gradually phased out, policymakers will need a multifaceted approach to address the issues COVID-19 amplified. The pandemic exposed many deficiencies in the Medicare program, while also presenting opportunities for improvement. Addressing these gaps will increase the value of the program and help it to be more effective and equitable for beneficiaries.





