The U.S. is facing a behavioral health crisis — a rise in mental health issues and substance use among adults and youth — which is exacerbated by a shortage of behavioral health providers. One way to extend the workforce is through integrated care, in which behavioral health specialists work with primary care and other providers to maximize each person’s time and expertise. Integrated care may be especially critical in rural or other areas where access to specialists is limited.
A common integrated care model utilizes a team located in the same facility, which allows for warm handoffs from primary care providers to behavioral health providers. However, many behavioral health conditions can be managed by primary care providers, especially if they can consult with specialists. Interprofessional consultation enables patients to receive care from their primary care providers while benefitting from specialists’ insights. The consultation can take place over the phone, via video, or in person.
Medicaid Will Now Allow Coverage for Interprofessional Consultation
On January 5, the Center for Medicaid and CHIP Services (CMCS) issued guidance changing its policy on Medicaid reimbursement for interprofessional consultation. Now, CMCS will allow use of federal matching funds for such consultations and has invited states to submit state plan amendments or waivers to implement this change. While the rule change applies to different types of consultations, the opportunities it provides in behavioral health are especially important. Being able to more easily consult with a behavioral health specialist (e.g., a psychiatrist or psychologist) may help primary care providers feel more knowledgeable and confident in their ability to treat patients with moderate or serious behavioral health needs.
The guidance details the scope of what Medicaid will cover and defines interprofessional consultation as:
a situation in which the patient’s treating physician or other qualified health care practitioner . . . requests the opinion and/or treatment advice of a physician or other qualified health care practitioner with specific specialty expertise . . . to assist the treating practitioner with the patient’s care without patient face-to-face contact with the consulting practitioner.
For example, a person enrolled in Medicaid may go to their regular primary care provider after experiencing a sudden change in their depression symptoms, after a period of relative stability. Without coverage for interprofessional consultation, the primary care provider would need to decide whether they could continue to manage that person’s behavioral health needs or refer her to a specialist, which could be appropriate in some instances but could also lead to fragmentation of care. Through interprofessional consultation, the primary care provider could confer with a behavioral health specialist about continuing to treat their patient’s depression and receive advice about referrals and coordination.
Policy Change Supports Range of Options for Integrated Behavioral Health Care
Medicaid coverage of interprofessional consultation provides a critical new path for states to expand equitable access to behavioral health care.
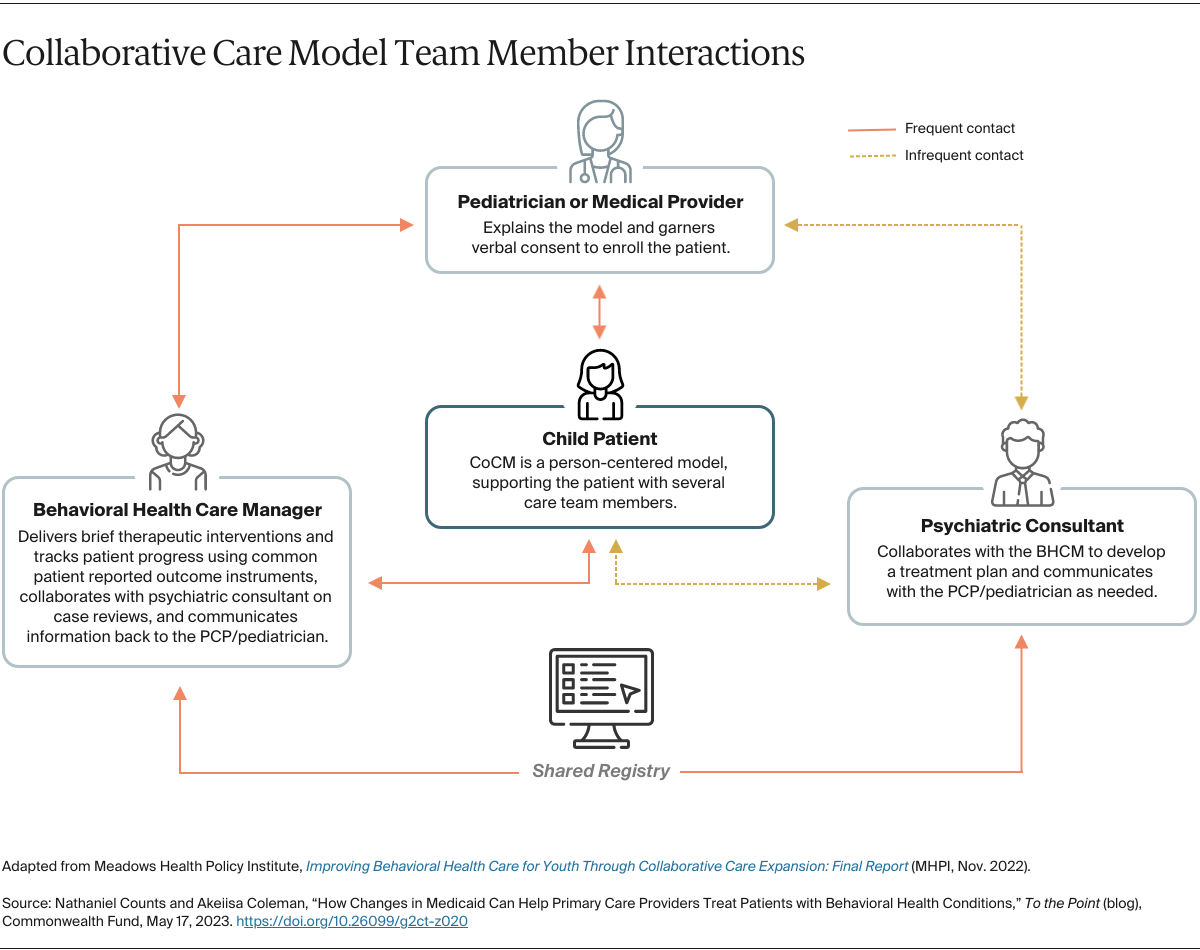
Medicaid already covers some integrated care models, such as the collaborative care model (CoCM), in which a primary care provider, behavioral health care manager, and psychiatric consultant work together under carefully defined roles. Under Medicaid’s previous coverage option for CoCM, the primary care provider billed for the entire episode of integrated care and had to work out a payment arrangement with the behavioral health specialist.
Under the new policy, the behavioral health specialist can bill independently for the consultation and the primary care provider can bill for the services they provide. Not only does separate billing allow for more straightforward administration, it supports more frequent consultations if needed. Separate billing also allows for consultations in settings where CoCM might not be applicable, such as emergency situations or one-off consultations.
Giving providers a range of options is critical, as evidence indicates that few people who would most benefit from CoCM now have access. The rule change also covers other critical activities. For example, billing for interprofessional consultation could support case review and consultations through Project ECHO, which connects primary care providers with specialists through virtual meetings. This model is frequently used in rural and frontier areas to enhance providers’ capacity to treat specific conditions (e.g., opioid use disorder).
Expanding Care to Those Who Need It Most
As noted, to leverage this policy change states must submit Medicaid state plan amendments and waiver requests that include coverage for interprofessional consultation. States should consider how billing for interprofessional consultation in Medicaid could support or extend their existing efforts to increase equitable access to care. They also should consider ways to promote equitable implementation of interprofessional consultation.
For example, many states have Child Psychiatry Access Programs that could now be sustained and expanded under this policy change. Child Psychiatry Access Programs offer centralized psychiatric consultation for providers serving children to support effective management of behavioral health in primary care settings.
On the other hand, many providers that could benefit from interprofessional consultation, such as those in rural and other underserved areas, will have trouble taking advantage of the coverage change without support for implementing new technologies and changing workflows. To promote equity, states should invest in infrastructure and training as part of the implementation, ensuring that integrated behavioral health care reaches those who would benefit the most.


