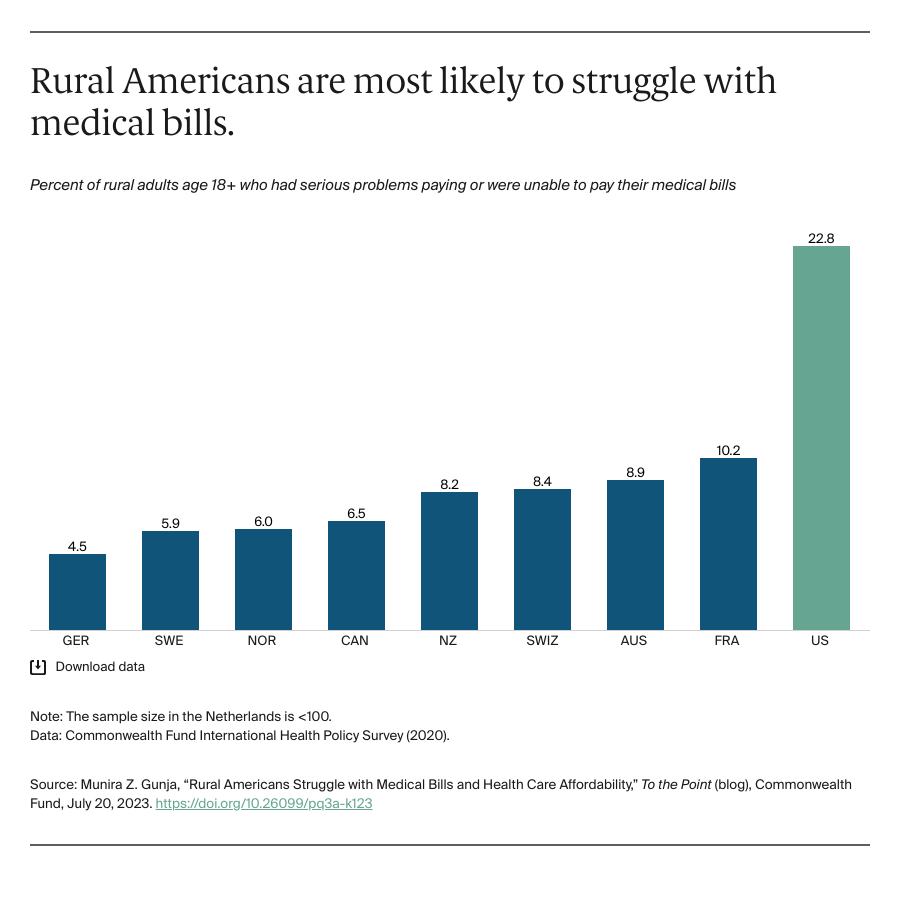
Prior research consistently shows that the high cost of health services in the U.S. affects consumers with or without insurance coverage, leading to higher medical bills and medical debt. The survey found that nearly a quarter of rural Americans reported either serious problems paying medical bills or an inability to pay altogether. Fewer than one of 10 rural adults in nearly all the other countries surveyed reported struggling to pay their medical bills.
What Can the U.S. Learn from Other Countries?
U.S. policymakers should look to other countries to determine the factors that contribute to geographic health disparities and policies and practices to improve health equity.
Guarantee every person has access to health insurance. The U.S. is the only country in this analysis without a universal health care system, leaving more than 10 percent of the rural population uninsured and nearly three of 10 underinsured.1 In all other countries, every resident, no matter where they live, has access to primary health coverage free of charge.
Location matters when talking about access to care. While having health insurance is necessary, the coverage itself is meaningless if rural communities lack an adequate health system, composed of doctors, pharmacies, and hospitals. In the U.S., there are over 4,000 rural areas with a shortage of primary care health professionals. Rural Americans are among the least likely to have adequate access to care compared to their counterparts in other countries. While the physician shortage is a global problem, some countries have made efforts to combat it. In the U.K, for example, one study found most rural residents have long commutes to their doctor offices. As a result, community pharmacies have been established throughout rural areas that allow patients to get same-day care for minor illnesses through the pharmacist. As a result, patients have greater access to primary care and can be treated more conveniently.
Use telehealth. Canada, which does not have significant disparities in health and health care between rural and urban residents, has used telehealth to reach more remote populations. Primary care physicians there are more likely to be satisfied with delivering care virtually compared to U.S. physicians, and there has been increased demand for telehealth use by physicians and the Canadian Medical Association Virtual Care Task Force. Canadian physicians have called for more training and payment models to support delivering care through telehealth. In the U.S., providing adequate care through telehealth is a continuous challenge as providers face reimbursement issues, which vary based on insurance type and state requirements. In addition, many rural communities lack access to the technology needed to effectively use telehealth services. While one study found that people in rural America are satisfied with telehealth, they are also more likely to report having technical problems accessing telehealth compared to those in nonrural areas.
Recruit and retain health care workers in rural areas. In Australia, over a 15 year period, the government created 19 clinical schools throughout the country that require at least one-quarter of students to come from rural areas, and at least one-quarter of students practice in rural settings for a minimum of one year. Other incentive programs, including health workforce scholarship programs and health insurance benefits for foreign medical workers, have been established to improve access to doctors in rural areas.
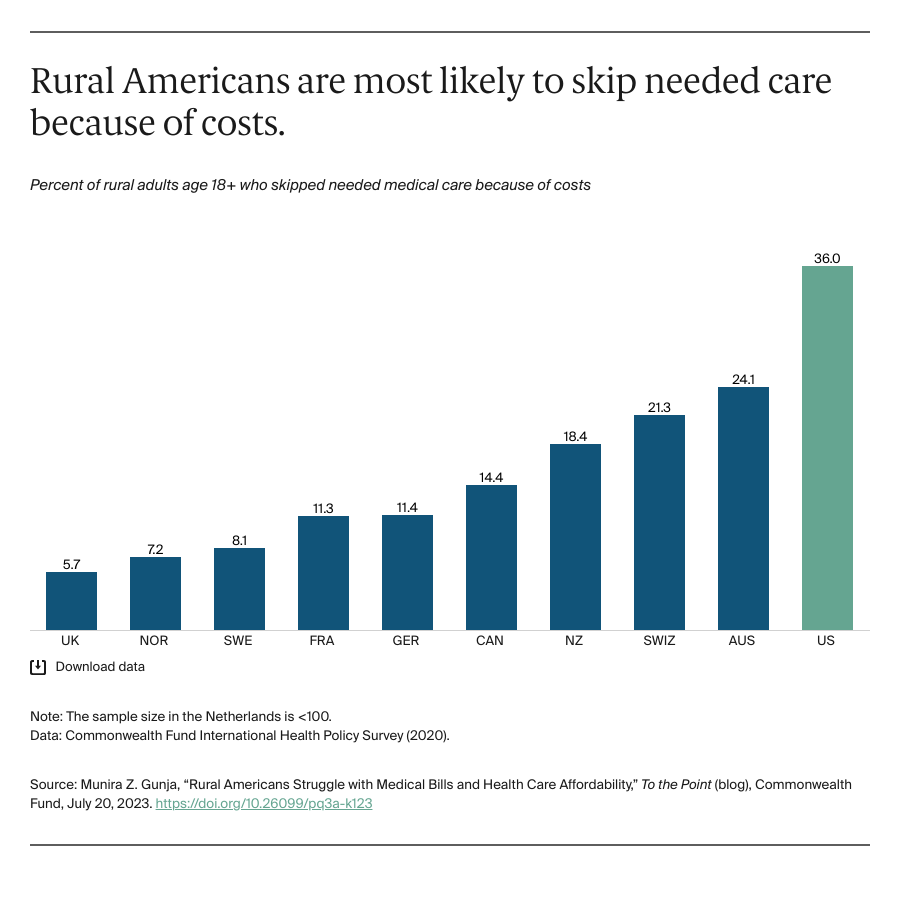
Rural Americans are more likely to report financial barriers to utilizing health care compared to rural residents in any other high-income country. With affordability problems preventing Americans from seeing their doctor, it is no surprise that rural Americans also are more likely to have higher rates of chronic conditions and some of the highest rates of mental health conditions. Other countries have been able to reduce these financial barriers. Adapting similar models can ensure rural populations in the United States get the health services they need while reducing health inequities.