Introduction
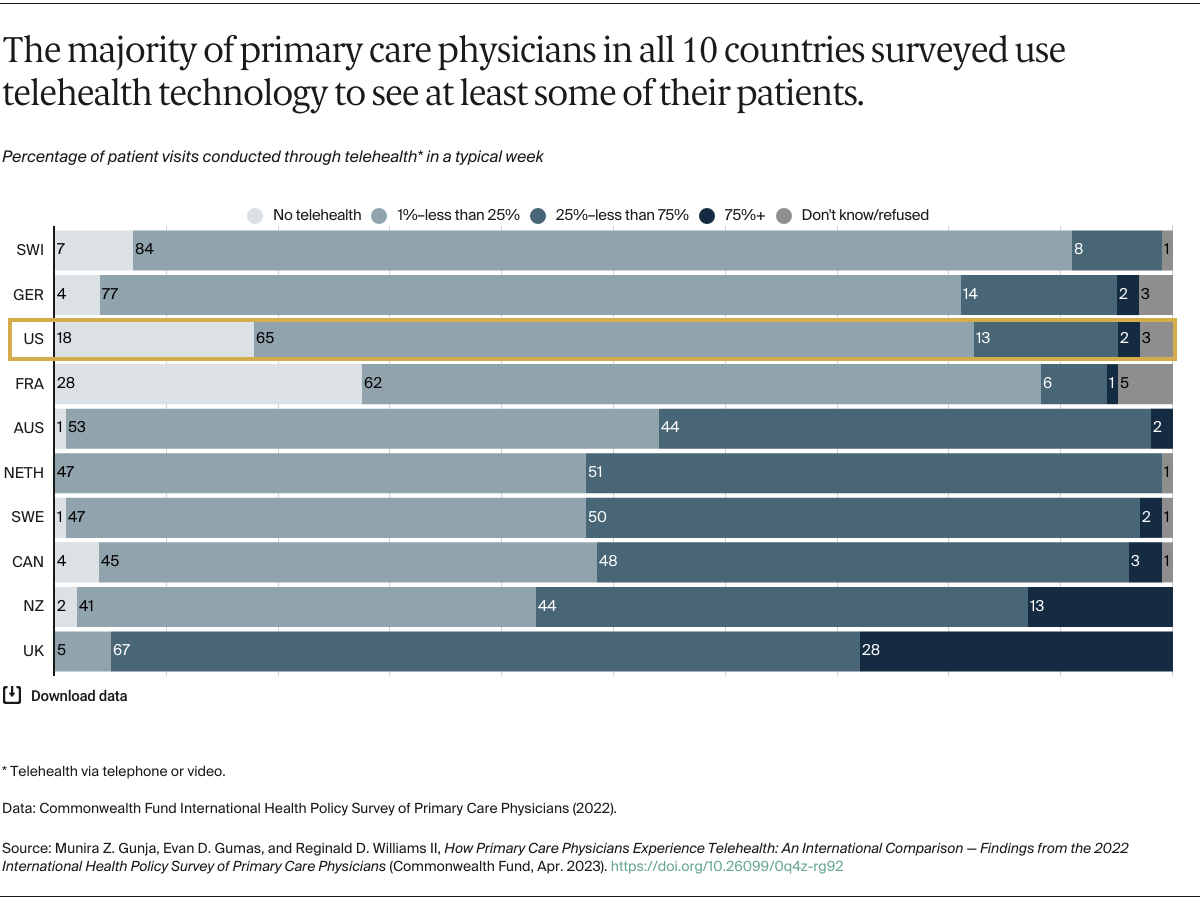
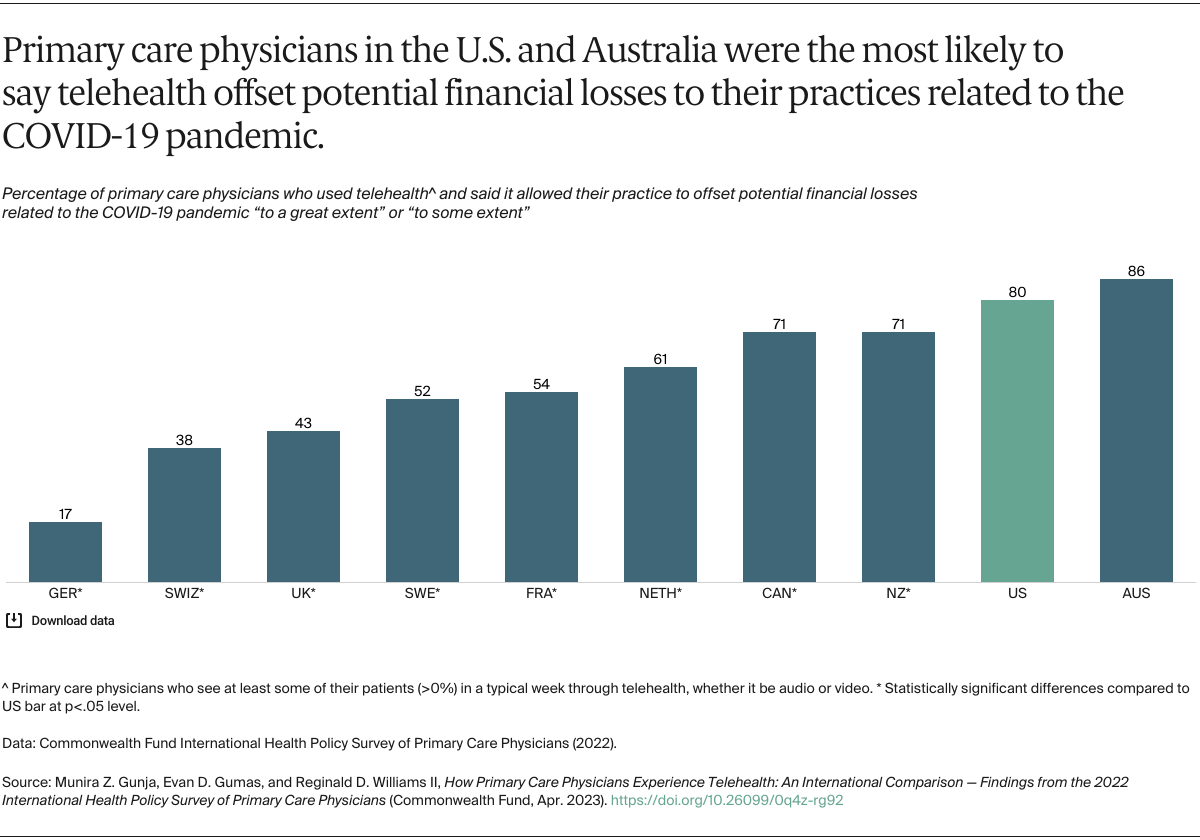
In the early months of the COVID-19 pandemic, lockdowns and social-distancing rules caused in-person primary care consultations to plummet.1 Many clinicians opted for telehealth — the provision of clinical and other health-related care by video or telephone — as an alternative to face-to-face office visits. Governments in many countries, including the United States, facilitated this shift by loosening regulations and enhancing payment and reimbursement for telehealth services.2
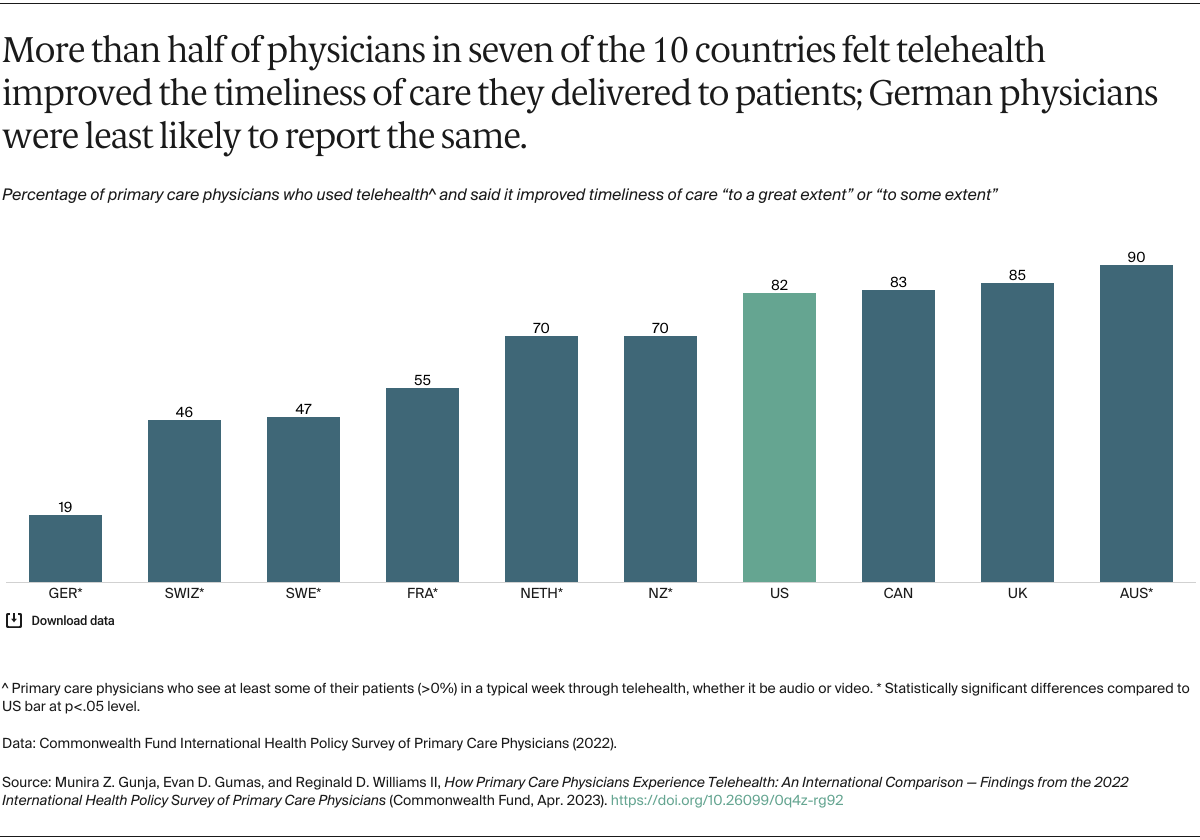
Telehealth’s popularity with patients during COVID-19 suggests it will have continuing utility beyond the pandemic.3 With the global shortage of primary care physicians and exposed inequities in access to health care, telehealth may turn out to be a better way to deliver critical health services to underserved populations.4
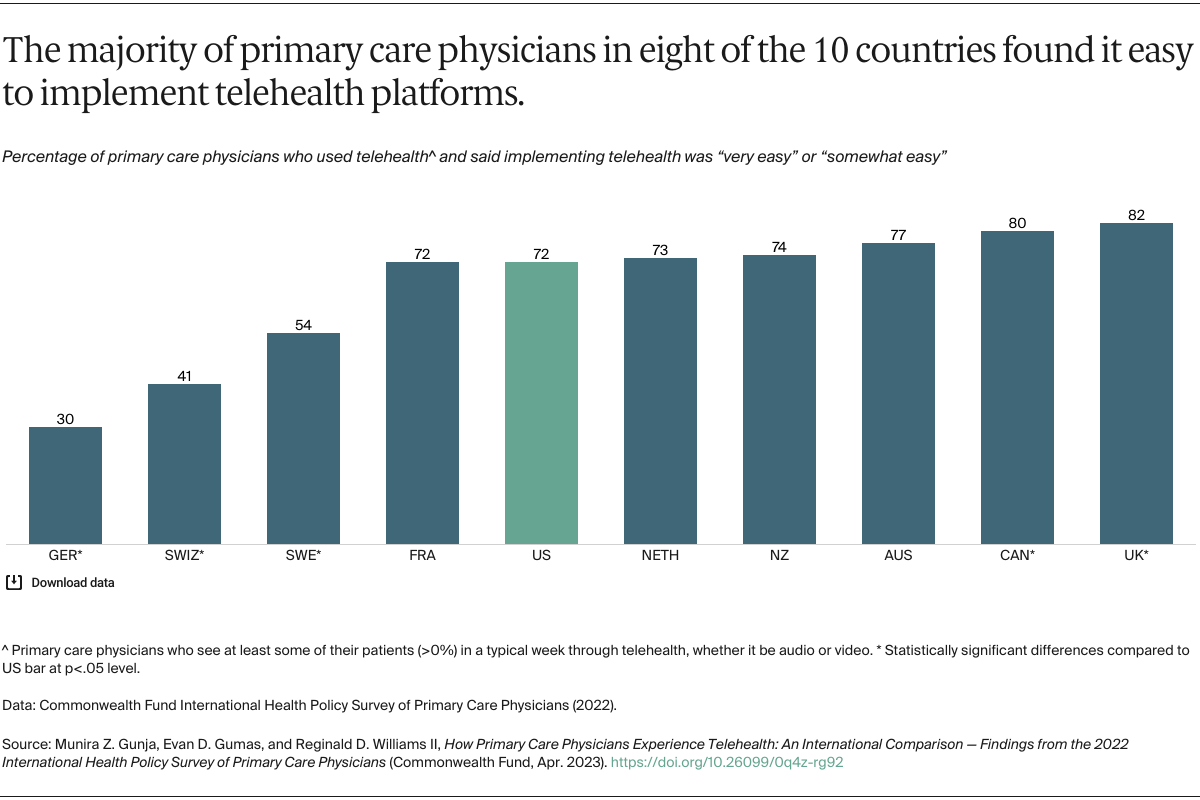
While there is a rich body of research describing the benefits and challenges of telehealth for patients, providers’ perspectives have been far less explored. Their experiences are critical to future policy decisions about financing, regulating, and possibly restricting telehealth services.5 This brief presents findings from the 2022 Commonwealth Fund International Health Policy Survey of Primary Care Physicians, conducted in 10 high-income countries from February through September 2022, to explore how primary care physicians view the ease of use and effectiveness of telehealth after the height of the COVID-19 pandemic. Our analysis is largely limited to those physicians who reported using telehealth, whether through telephone or video, at least some of the time.