During national health emergencies like the COVID-19 pandemic, a robust primary care system plays a critical role in triaging, testing, and educating patients. The U.S. primary care system was underprepared for the pandemic, largely because it had been weakened by chronic underinvestment and workforce shortages. In turn, our primary care system took massive blows from the pandemic: drops in visit volume, decreased revenue, challenges with rapidly adapting to telehealth, and provider burnout.
As we enter the third year of the pandemic, it is critical to assess the impact of COVID-19 on primary care and implications for the future as providers continue to struggle to care for patients and maintain their practices.
Many practices have begun to financially recover, but some still struggle.
In the spring of 2020, primary care faced significant financial losses as patients stopped seeking in-person care. At the time, researchers estimated that primary care would lose $15.1 billion as a result of the pandemic, driven largely by minimal and uncertain telehealth reimbursements and decreased in-person visits. In early 2020, a primary care provider polled in a weekly survey conducted by the Larry A. Green Center, a nonprofit research institute focused on primary care in the United States, said, “We are setting up telehealth as quickly as possible with no idea how much or if we will get paid.”
By the summer of 2021, primary care providers began to recover financially, owing to an influx of federal funding and expanded telehealth reimbursements. Yet many primary care practices, especially small and independent ones, still experienced substantial financial burdens. A third (32%) of these providers polled by the Larry A. Green Center reported that as of September 2021 their practices had not recovered financially.
A year ago, experts predicted the pandemic would accelerate the trend of small practices consolidating with larger health systems, heightening concerns about increased prices without improvements in quality. Evidence suggests COVID-19 has in fact accelerated growth in acquisitions of independent practices and physicians, with a sharp uptick following the start of the pandemic.
Telehealth has been a powerful tool during the pandemic, but providers are uncertain about its long-term potential.
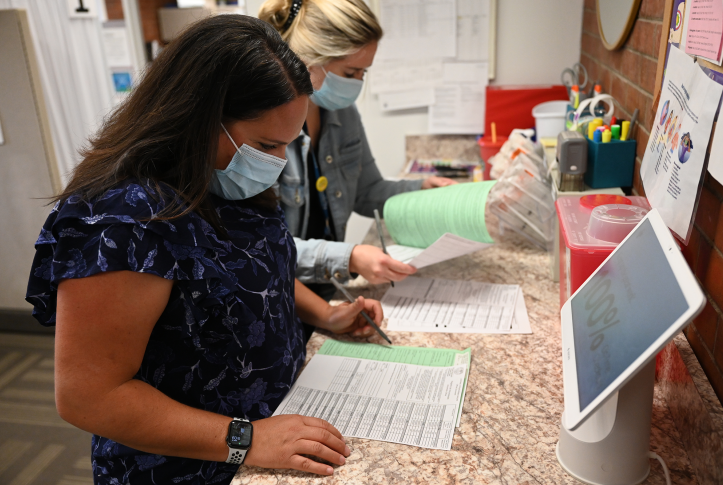
As in-person visits dropped, providers rapidly shifted care online, many for the first time. In the first half of 2020, telehealth made up 20 percent of primary care visits, compared to 1 percent a year before. But the surge in telehealth visits brought more than financial challenges, with widely varying telehealth capabilities and provider knowledge. In addition, not all services are considered appropriate for telehealth, and access to telehealth platforms varies by patients’ age and location.
As time went on, providers became increasingly comfortable providing telehealth. Private payers, Medicare, Medicaid, and individual states expanded their reimbursement policies. Many providers attribute their continued telehealth use to better reimbursement but are concerned what the end of the public health emergency will bring for telehealth policy, especially since many implementation challenges remain.
COVID has greatly stressed primary care providers, but it is unclear if it has caused a mass exodus, as predicted.
The pandemic has led to significant primary care clinician burnout. In April 2021, just over one year into the pandemic, 71 percent of primary care providers said their level of burnout was at an all-time high (compared to 33% in May 2020). Providers faced many of the same anxieties as their patients, coupled with heightened concerns about COVID transmission while at work, financial losses, and potential practice closures. Reflecting on the pandemic’s emotional toll, one physician said “it’s impossible to experience [COVID-19] on the frontlines and not come away with feelings of awe and dread for the entire health care workforce.”
The financial and emotional strain of COVID certainly had the potential to worsen the primary care workforce shortage, but the impact may not be as bad as feared. There was concern the pandemic would lead older providers to retire early or younger ones to leave the field. By the fall of 2021, 44 percent of practices were facing clinician turnover and 45 percent of providers reported knowing providers who had quit or retired early. However, the 2021 edition of the Association of American Medical College’s primary care physician workforce study predicted future shortages won’t be as great as had been predicted in past studies. This is in part because of indications that more primary care physicians are being trained, increased federal funding for their training, and more loan-forgiveness programs.
The U.S. primary care system has been resilient in the face of COVID-19 but needs continued support.
As we enter the third year of COVID-19, policymakers should consider ways to bolster the U.S. primary care system to ensure it is prepared for future emergencies and equipped to handle the long-term impacts of COVID-19, including treating patients who delayed care and those struggling with long COVID. Experts are increasingly coalescing around a core set of policy reforms to strengthen primary care, including reforming how we pay and how much we pay for primary care, ensuring telehealth flexibilities last beyond the public health emergency, and increasing investments to build the primary care workforce.