Surveys and studies have documented that people seeking in-network care for behavioral health conditions encounter serious access problems. This longstanding issue has been exacerbated by an increasing need for these services and shortages of behavioral health providers, particularly in rural areas. Addressing these challenges requires a multipronged approach that includes bolstering provider capacity while also ensuring that the providers who are available are part of plan networks. Indeed, a key barrier to access is the large share of available providers who don’t participate in any network. To improve access and help people get the care they need, state and federal policymakers could begin by creating strong standards for behavioral health networks and ensuring plans are constructing their provider networks in ways that meet federal standards for covering mental health care on par with other care.
Federal Standards Set a Floor
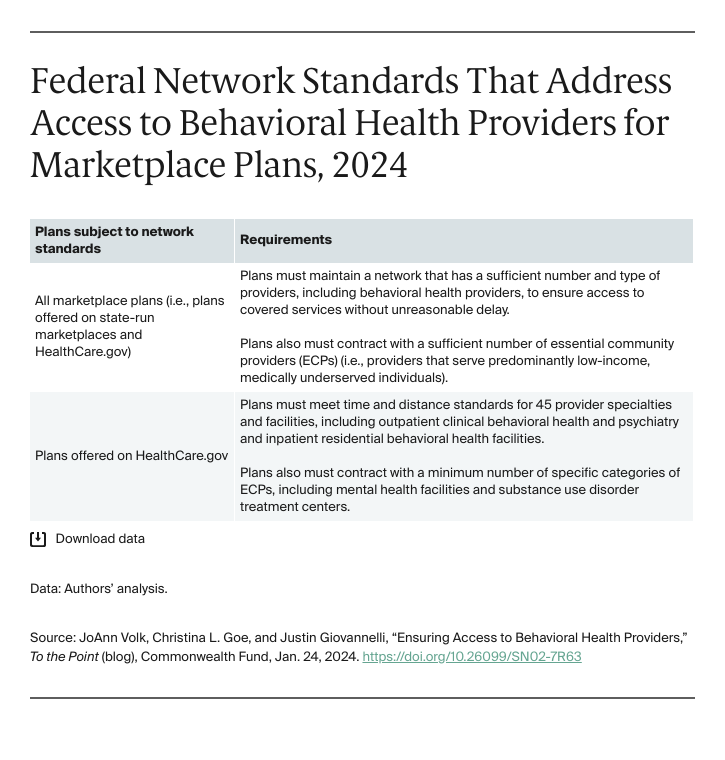
The Affordable Care Act (ACA) sets minimum provider network standards that all marketplace plans must meet to guarantee access to covered services, including behavioral health. Beginning in 2023, federal regulators strengthened standards for plans offered on HealthCare.gov by requiring them to satisfy numerical measures of access — maximum time or distance to travel to an appointment, for example — for certain providers. In addition, those standards were extended to a small subset of behavioral health providers. Recently, federal regulators proposed that these standards should become minimum requirements for all marketplace plans (including those sold through the state-run marketplaces), with states still able to establish rules that do more to protect consumers.