News of growing health disparities between rural and urban Americans prompted Transforming Care to focus on what’s happening in rural health care today. What we found was surprising: While there is much to worry about—including a greater risk of dying from preventable causes and worse access to care—there are also many signs of innovation, including bold experiments in organizing and financing care delivery, making services more accessible, and addressing the social determinants of poor health. This issue focuses on these bright spots—places where policymakers, providers, and community organizers are seeking to transform their health care systems to better serve residents.
By Martha Hostetter and Sarah Klein
Forty-six million Americans—some 15 percent of the U.S. population—live in rural areas of the country.1 Data from the Centers for Disease Control and Prevention show they are more likely to die from the five leading causes of death—heart disease, cancer, unintentional injuries, chronic lower respiratory disease, and stroke—than residents in urban regions and that a greater percentage of rural deaths may be preventable.2 Gains in life expectancy among urban and rural Americans, which once tracked fairly closely, began to diverge in the 1990s. By 2009, the life span of residents of large cities was 2.4 years longer; for poor and black rural residents, life expectancy was what urban rich and urban whites enjoyed four decades earlier.3
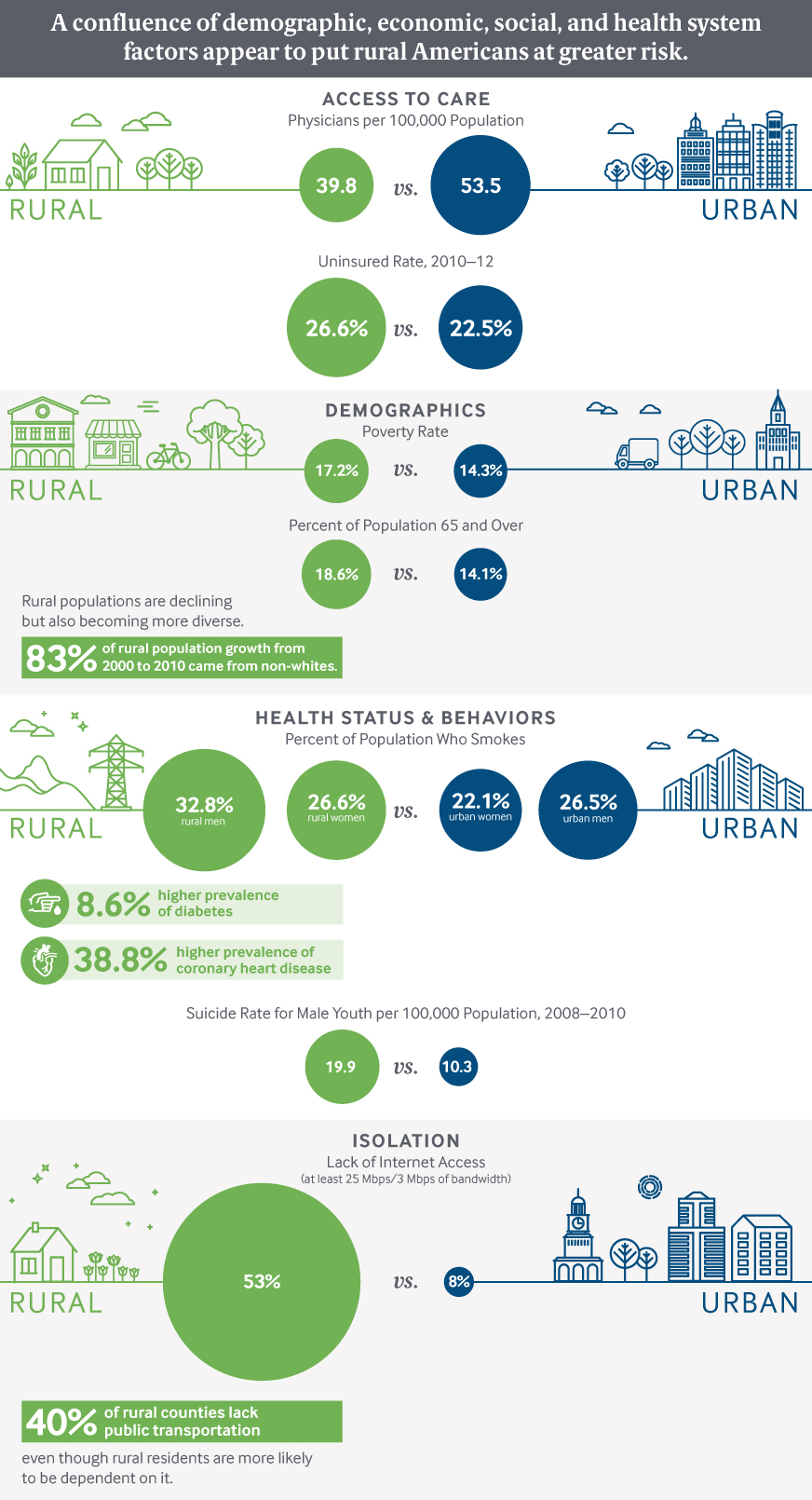
“Rural America is a unique health care delivery environment,” says Alan Morgan, CEO of the National Rural Health Association, a nonpartisan organization with more than 21,000 members. “You have an elderly population, you have a sicker population, and you have a low-income population. Yet you have the fewest options available when it comes to seeking care. It’s a perfect storm.”
But for all these challenges, Morgan and other experts say some rural communities have begun to innovate, adopting new care delivery and payment models to address long-standing workforce shortages and population health needs.4
Strategies to Shore Up Critical Access Hospitals
A key area of focus has been shoring up critical access hospitals—facilities with no more than 25 beds that offer acute care in communities where the next hospital is generally more than 35 miles away.5 There are roughly 1,300 of these federally designated hospitals nationwide, nearly all in rural communities. They receive cost-based reimbursement to reduce their financial vulnerability and keep essential services, including 24/7 emergency care, in rural communities. But despite this support, 80 rural hospitals have closed since 2010 for a slew of reasons: financial losses from declining inpatient volume, changes to federal and state reimbursement, difficulty in recruiting physicians, inability to keep up with new technologies, reductions in disproportionate share payments, or some combination of these forces.6
Rusk County Memorial Hospital, a critical access hospital in Ladysmith, Wis., in the northwestern part of the state, lost six physicians between 2010 and 2013—over half of its primary care workforce—in part due to competition from a major medical group that opened its own hospital 47 miles away.


Using Global Payments to Enable Transformation
Pennsylvania is implementing an entirely new payment model for its 30 rural hospitals, half of which are struggling from loss of inpatient revenue, according to Karen Murphy, the state’s Secretary of Health. To help them succeed in an environment in which payers are trying to reduce acute care, Pennsylvania is launching a global payment model under which critical access and other rural hospitals will receive a set budget for all inpatient and hospital-based outpatient services delivered for patients covered by Medicare, Medicaid, and some private payers. The first six hospitals will pilot the model next year.
The amount of the global payments will be based on each hospital’s revenue from the previous year. The hospitals will share in any savings they achieve from reducing spending on potentially avoidable utilization.8 The goal, according to Murphy, is to create incentives for hospitals to control costs through better coordination of patient care and use the savings to address population health issues. “We know our health outcomes are lower in rural communities and want to develop systems that really support chronic disease management, behavioral health, and efforts to help with the opioid crisis,” she says.
The Centers for Medicare and Medicaid Services (CMS) is providing waiver authority to enable this experiment, as well as a $25 million Center for Medicare and Medicaid Innovation grant to fund a rural health redesign center to provide hospitals with data analytics and other support.
At least three large private payers have signed on, Murphy says, though it took some convincing to persuade them they will not be paying for the same hospital admissions twice but rather for the health of the community. “We are shifting the conversation from utilization to health,” she says.9
Banding Together to Pursue Value-Based Care
In 2015, Eastern Maine Healthcare Systems, an integrated delivery system based in Brewer, Maine, helped launch the Beacon Rural Health ACO, an accountable care organization made up of five critical access hospitals, including three from its own system and two independent community hospitals. The five hospitals used the advance payments they received from CMS under the Shared Savings Program to create a translational information technology (IT) system to share data. Each month, they evaluate their performance and discuss improvement approaches including redesigning workflows to increase health screenings and immunizations, says Mike Murnik, M.D., chief medical officer of Blue Hill Memorial Hospital, one of the five ACO participants. “It’s allowed us to shake out what works best and spread that among practices,” Murnik says. With the ACO funding, Blue Hill has also hired nurse care managers to assist with care transitions for high-risk patients, including those with heart failure and chronic obstructive pulmonary disease. Medical assistants screen patients for issues like food insecurity and refer them to community nonprofits for help.
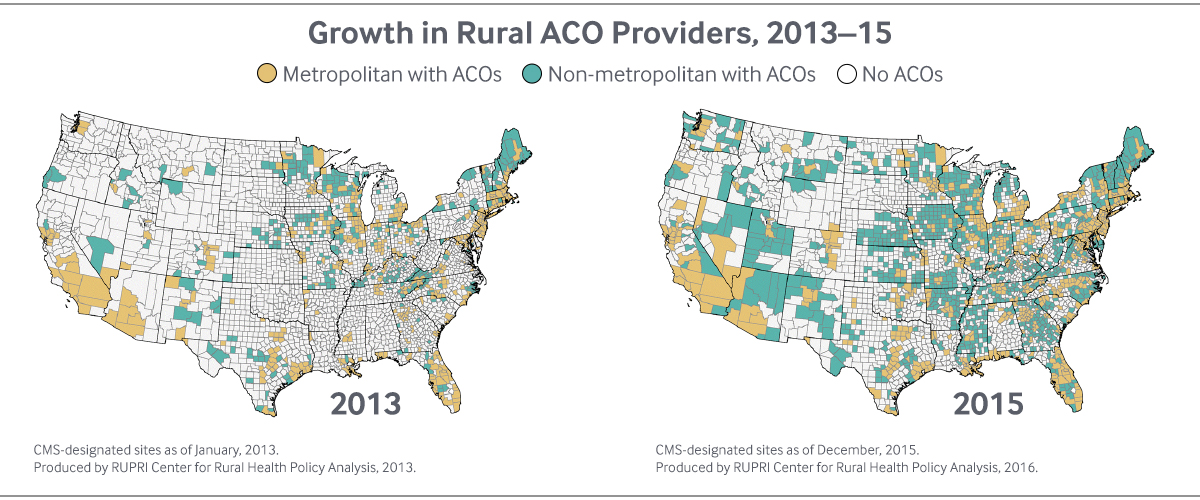
On a national basis, small, physician-led and rural ACOs have achieved greater success than other organizations participating in Medicare’s Shared Savings Program. The 35 ACOs that participated in its Advance Payment track—which provided upfront funds for such providers to invest in IT and other systems needed to function as an ACO—achieved 21 percent of all savings in the Shared Savings Program, even though their patients represented only 5 percent of beneficiary years.10 “The strength in rural communities is primary care—and the ACO model works best from a primary base,” says Keith Mueller, head of the Department of Health Management and Policy at the University of Iowa and director of its Center for Rural Health Policy Analysis.
Value-based care is the best business model rural providers have seen in a long time. It's bringing new life to the community, new jobs, and new revenues.
Lynn Barr, CEO of Caravan Health, a management services company based in Kansas City, Mo., that provides guidance and technical assistance to rural health care organizations that want to enter into value-based reimbursement arrangements, says part of these organizations’ success is attributable to the fact that many rural providers have longstanding relationships with their patients, making it easier to engage them. “They are doing care coordination at the supermarket and at the soccer field,” Barr says.
Caravan supports 159 rural health providers—both hospitals and clinics—that in 2015 organized themselves into 23 ACOs in Medicare’s Shared Savings Program.11 It takes an unusual approach to the problem of small numbers in rural communities: to form what Caravan deems to be a sufficient ACO cohort (about 10,000 patients), it aggregates patients from across unaffiliated providers, sometimes in different states. One of its most successful ACOs includes patients from Mississippi and the state of Washington. Caravan then offers the providers coaching, technical assistance, software, and data analytics. The providers must hire a nurse care coordinator to implement new approaches, which focus on wellness visits, chronic care management, integration of behavioral health into primary care, improving dementia care, and ensuring safe care transitions. Half of the ACO participants have been able to reduce costs within nine months, Barr says. Some of the gains are from picking low-hanging fruit—for example, helping patients who use the ED every week because of anxiety or who have out-of-control diabetes, she says. “The other part is they are really nimble and able to adapt very quickly to get the whole health system around the table.”
Addressing the Social Determinants of Poor Health
Rural health providers are also partnering with community leaders to improve residents’ health by addressing the effects of poverty, isolation, and addiction. But it can be a challenge to convince rural residents to accept help, says Pam Guthman, clinical assistant professor of community/public health nursing at the University of Wisconsin and the former head of a community action agency in Ladysmith, Wis.12 “Rural communities tend to draw an invisible line around themselves because they view themselves as self-sufficient,” she says. This isolation can obscure problems that are endemic, such as homelessness, drug and alcohol abuse, poor nutrition, and deteriorating housing, she notes.
To make headway, some communities have involved the leaders of schools, churches, and other community institutions to make them aware of problems and have invested in finding solutions. One example is Project Lazarus, a nonprofit based in Moravian Falls, N.C., that has developed a community-based approach to reducing opioid abuse (see our Q&A with Fred Wells Brason II, president and CEO of Project Lazarus).
Helping High-Need Patients
The Southeast Health Group, a community behavioral health clinic, tapped health navigators to reach out to high-needs patients in its rural and frontier corner of Colorado, near the Oklahoma and Kansas panhandle.13 The clinic serves nearly 47,000 people across 10,000 square miles, providing both behavioral health and physical health care services. The clinic’s providers found such patients often needed hands-on support to help them manage their conditions and stabilize their lives. To provide this, Southeast Health Group applied for and won a $1.4 million grant from the Center for Medicare and Medicaid Innovation to hire navigators to help patients who accrued $10,000 or more in Medicaid services in a year, accepting referrals from its own providers and from Medicaid, a local FQHC, and the ED at the local hospital.14

“We gave the navigators carte blanche to do anything they needed to do to help the patient succeed,” says Nancy King, Southeast’s development director. Transportation proved to be a major hurdle for many patients. “Our navigators drove over a million miles over the three-year project,” taking patients to their regular clinic visits or specialist appointments in Pueblo (120 miles away) or Denver (175 miles away) and to pick up prescriptions and healthy food, using the time to get to know patients and offer them advice and coaching.
Health navigators served 639 patients over three years. Along with driving and coaching, they secured mental health treatment and housing for homeless patients, helped those with unmanaged diabetes create health journals, and convinced a patient who had experienced multiple rapes to overcome her fears of the hospital environment and pursue a necessary operation, among other activities. Among those receiving such support, there was a nearly 20 percent reduction in average per capita emergency department visits, from a baseline of 0.56 visits per person in 2012 to 0.46 visits per person in 2015. While per capita Medicaid costs dropped among all the high users tracked during this period, savings were much greater among those receiving services from the navigators.
Channeling Savings into Community Health
In Central Oregon, a region that’s home to college students, ranchers, and Native Americans, efforts to improve community health are funded by savings achieved from better coordinating care for Medicaid beneficiaries. Based on a joint agreement, the region’s coordinated care organization—a network of medical, dental, and other providers that collaborates to care for Medicaid beneficiaries—agreed to take only 2 percent annual profit and distribute the rest to its governing body, the Central Oregon Health Council, to be used for communitywide health improvement efforts (i.e., not just those that benefit Medicaid beneficiaries).15 To carry out this agreement, the council convenes health systems leaders, providers, consumer advocates, representatives from local schools and nonprofits, and others to determine how to spend the funds to address substance abuse, high rates of diabetes, tobacco use, and other problems identified through its Regional Health Assessment. For example, one project aims to reduce the incidence of low–birth-weight babies by coordinating prenatal care and support services for high-risk pregnant women.

Pursuing Economic Health and Physical Health Simultaneously
A public–private partnership in Eastern Kentucky known as SOAR (Shaping Our Appalachian Region) seeks to strengthen the local economy, diversifying away from its historic dependence on coal by retraining displaced workers, investing in broadband networks, encouraging tourism, and promoting health.16 Appalachian residents are among the sickest in the nation, with diabetes, obesity, and substance abuse endemic. William Hacker, M.D., the former state health commissioner and chair of SOAR’s Community Health Advisory Council, says the region’s health problems are exacerbated by its mountainous terrain and a history of boom-and-bust cycles. “We have food deserts, we have a lack of convenient walking areas and trails, and so the infrastructure works against good health habits,” he says. “And there’s a segment of the population who are fatalistic about their health—who would like to do better but who find the day-to-day challenges of living overwhelming.”
With the help of two public health officers from the Centers for Disease Control and Prevention, counties across the Appalachian region are encouraging healthy eating habits and physical activity and helping people identify and manage diabetes. In one effort, SOAR hosted a Health Hack-a-Thon to develop solutions.17 A team of Pikeville High School students won in the obesity category for its Simple Health 5-5-5 prototype app, which would encourage people to drink five glasses of water, eat five servings of fruits and vegetables, and walk five minutes every day.
Looking Forward
These experiments in expanding rural workforce capacity, leveraging value-based payment, and addressing the social determinants of poor health in rural communities are still nascent, and the needs are daunting. Local champions and collaboration, as well as support from state and federal governments, have enabled these efforts. To build on them, it will be important to learn from promising approaches and to secure stable investments in the health of rural America.






