For diabetes patients who want reminders about when to take their insulin, or young mothers looking for tips on nursing, new digital technologies — from apps and text-messaging services to remote monitoring tools and wearable sensors — are making life easier and even leading to better outcomes.
One nonprofit focused on a mobile technology for lower-income patients, called CareMessage, has found that when a free clinic sent patients with diabetes two daily questions and two weekly educational messages over 12 weeks, the patients had lower blood glucose levels than they did before the texts. CareMessage is just one of a growing number of providers using digital tools to try to engage lower-income patients in their own care, and to identify their needs and tailor services to meet them.

There are millions of low-income Americans who could likely benefit from such technologies. Medicaid is the nation’s largest insurer, covering one in five Americans. In certain parts of the country, it covers an even larger proportion of people. In the Bronx, 71 percent of the population is covered by Medicaid. And the number of Medicaid beneficiaries nationwide is likely to grow with recent Medicaid expansion ballot initiative wins and gubernatorial victories among expansion supporters in five states.
See also: The Time Is Now: The Case for Digital Health Innovation for the Poor and Underserved
“Medicaid expansion under the Affordable Care Act created an opportunity like never before,” said Vanessa Mason, who cofounded P2Health Ventures, a public health tech fund, about the low-income market for digital health tools.
Past Obstacles to Digital Health Tools for People on Medicaid
Yet, to date, much innovation in health care technology has been developed for middle- and high-income consumers who obtain health coverage through their employer or purchase it on the private market. Marketing to people with Medicaid has not been of interest to many digital health entrepreneurs because, at first glance, innovating for the poor doesn’t seem to make financial sense. Other reasons digital health entrepreneurs have focused on the commercially insured market are because it does not face the budget scrutiny of a public program, and patients with private plans are perceived as more technologically savvy.
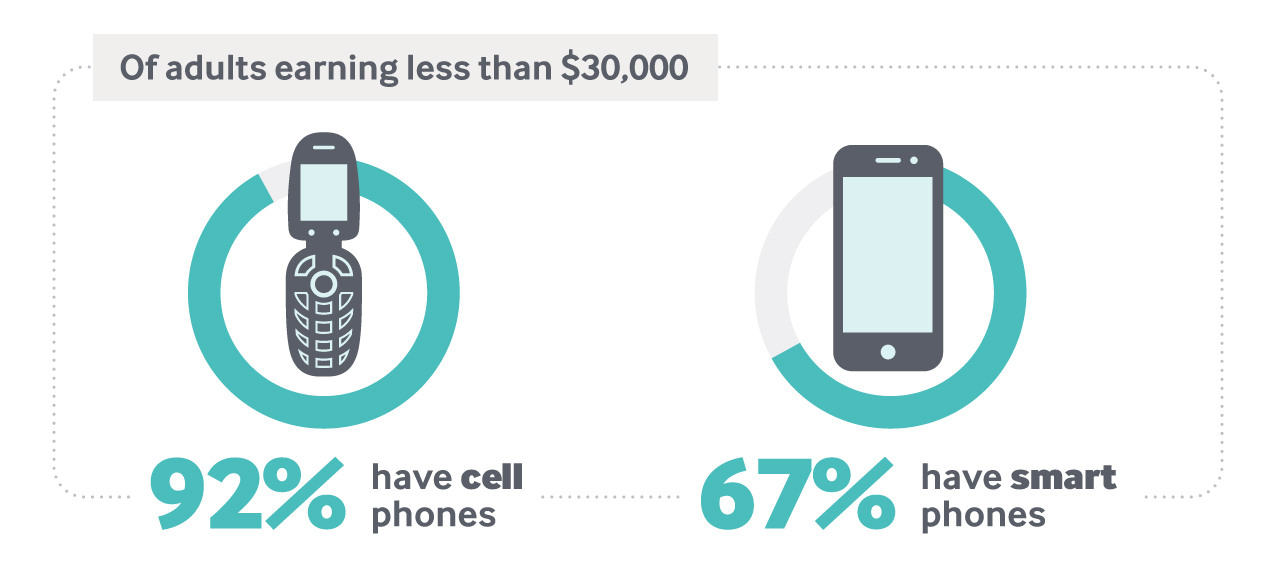
For example, there has been a misperception among health care entrepreneurs that low-income people may not have cellphones or smartphones with which to access digital tools. In fact, 92 percent of adults earning less than $30,000 have cell phones, and 67 percent have smartphones. Another reason tech companies have been wary is that Medicaid pays providers lower reimbursement rates than commercial health plans or Medicare.
“People think of Medicaid as a low-margin business, which it is for providers and health plans, but not necessarily for technology companies,” explained Julian Harris, president of the health management services company CareAllies, and former associate director for health in the White House Office of Management and Budget. A technology company could still see good margins for profit because many digital services can be easily scaled to reach more people, whereas a physician can only see a certain number of patients in a day.
Recognizing Opportunities
But tech companies’ perceptions of people with Medicaid may be changing, as entrepreneurs become more familiar with the large, relatively untapped market of patients who depend on the health care safety net. “Not to say there aren’t barriers, but there’s a business case to be made because there is a vital, urgent customer need,” said Mason of P2Health Ventures.
One aspect of Medicaid is both a challenge and an opportunity for digital entrepreneurs: Each Medicaid program is distinct, because states have great flexibility in how they run their programs and are encouraged to test new approaches both in coverage and in how care is delivered to patients. “People always say, ‘If you’ve seen one Medicaid program, you’ve seen one Medicaid program.’ But there are also 50 shots at gold, certainly in terms of going directly to the state and trying to find some providers to run pilots with,” Harris said.
Not to say there aren’t barriers, but there’s a business case to be made because there is a vital, urgent customer need.
Further, unlike the federal government, states must balance their budgets each year. Since Medicaid accounts for an increasing portion of their budgets, states are often looking for solutions that can help rein in costs. For example, a small number of Medicaid patients with complex needs account for a large portion of health care spending. If it becomes possible to avert even one ED visit or hospital admission by digitally monitoring diabetes, disabilities, or a behavioral health issue, it could provide a return on investment for a provider or a payer responsible for their health costs.
On the other hand, many people on Medicaid just require help at certain times — like during pregnancy and delivery. Developing tools to support pregnant mothers and healthy deliveries would disproportionately impact Medicaid spending, said Harris, because Medicaid pays for 50 percent or more of all births in 24 of 50 states.
CityBlock Health is a new start-up building digital health platforms for people on Medicaid or Medicare in city neighborhoods that have typically lacked good health services. CityBlock assigns integrated care teams to patients in historically underserved communities, and launched its first “Neighborhood Hub” in Brooklyn in July 2018. Patients can use their smartphones, tablets, or computers to reach their care team on CityBlock’s tech platform, called Commons. CityBlock’s tech component aims to act as digital extenders of clinicians, making it possible to provide in-person care in a more targeted, financially feasible way.
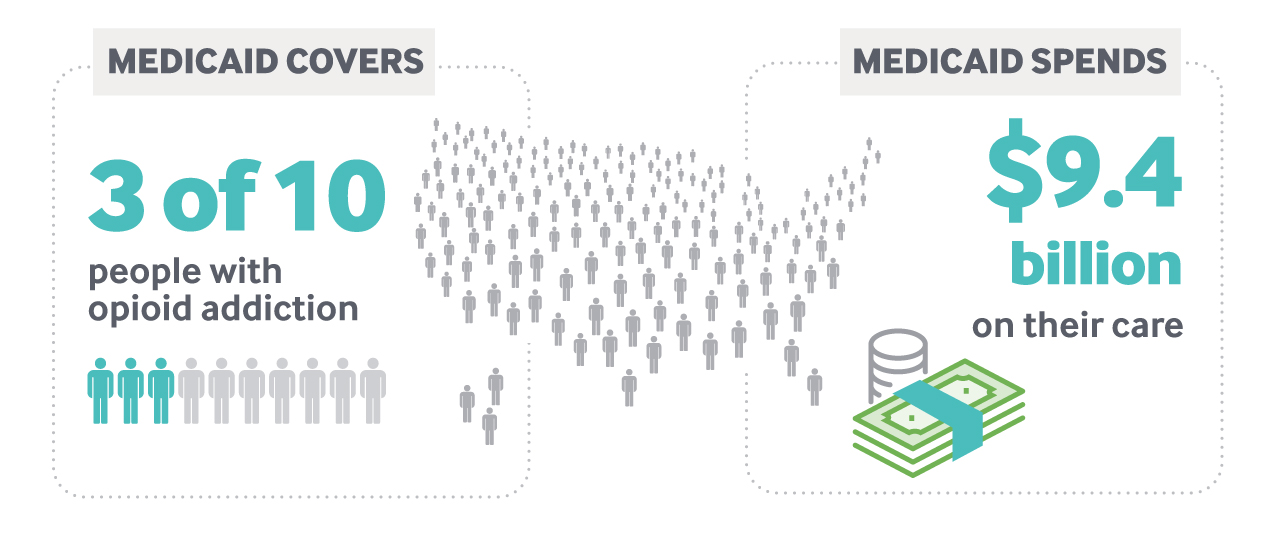
In the case of opioid addiction, which payers and policymakers alike are desperately trying to address, Medicaid offers a significant market opportunity for technology companies: It covers three of 10 people with opioid addiction, and spends $9.4 billion on their care. The federal government is already acknowledging the potential of technology to address the opioid epidemic: in December 2017, the U.S. Department of Health and Human Services hosted its first “code-a-thon,” awarding $10,000 prizes each to the three most promising ideas. One winning team developed a model to track overdoses in real time, making it easier for first responders and health authorities to allocate resources.
If companies pursue these opportunities, states could benefit, and patients could see improvements in care. For patients, apps and other digital tools that increase engagement and care coordination have numerous benefits. For example, remote care managers — telehealth programs that provide remote monitoring, care, and resources — help patients with chronic diseases manage their conditions themselves between office visits and provide real-time advice to avert emergency department visits. And tools that connect patients to community services and supports reduce loneliness and improve the nonhealth factors that impact health and quality of life.
Opportunity for People and Profits
To be sure, digital health tools specifically designed to meet the needs of low-income patients are still few and far between, and on their own won’t fundamentally shift the way people covered by Medicaid receive care. But innovating for Medicaid patients is a first step, and gives entrepreneurs an opportunity to reach underserved patients. This is key to ensuring that “along with all the fitness trackers and all the attention that’s being paid to the employer population, there is similar attention for low-income or vulnerable populations,” said Dan Gebremedhin, a principal at the health care technology venture capital firm Flare Capital Partners.
Technology has the potential to reduce barriers to care and provide information in appropriate ways — in terms of culture, language, and medical literacy. It can remotely monitor and intervene, and connect with people not currently accessing the health care system, thereby decreasing health disparities. With over $550 billion being spent on Medicaid each year, digital health entrepreneurs need not stay away for lack of funds. For entrepreneurs, this creates an opportunity to do well and do good.