Introduction
The Geriatric Resources for Assessment and Care of Elders (GRACE) model was created for patients like Elizabeth, a patient with cognitive impairment and diabetes. After she was discharged home from the hospital after a stroke, her elderly husband found his new role as a caregiver to be challenging.
Carrie Ortwein, a nurse practitioner, and Olivia Dole, a social worker, were assigned to work with Elizabeth as part of a GRACE care team at Indiana University Health Medicare Advantage Plan. During home visits, they educated Elizabeth’s husband about her cognitive impairment and provided support for her other medical and social needs so she could continue living at home safely and independently.
The GRACE model was developed by geriatrician Steven Counsell, M.D., at Indiana University School of Medicine to help primary care providers overcome the limitations of delivering care to older patients in an outpatient setting.1 Exhibit 1 outlines the hallmarks of the model. “GRACE was designed to bring a comprehensive geriatric focus to what is essentially an intensive patient-centered medical home (PCMH) model for patients with complex needs,” he says.2
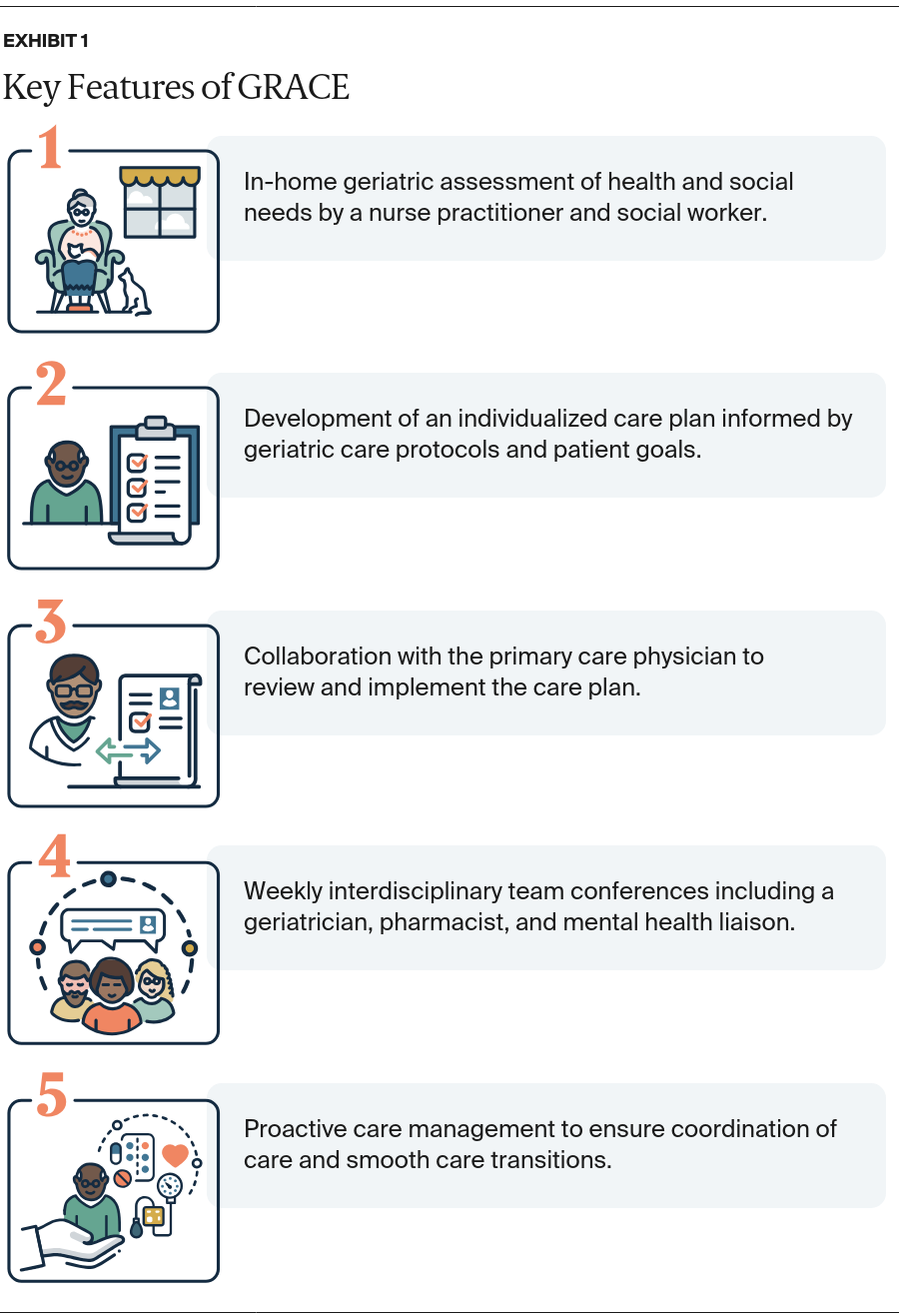
The GRACE model augments the PCMH, a collaborative primary care model designed to improve care coordination and patient access, with in-home visitation by a care team. This team is supported by geriatric protocols and other professionals who understand the unique needs of aging patients and offer recommendations for care and follow-up.
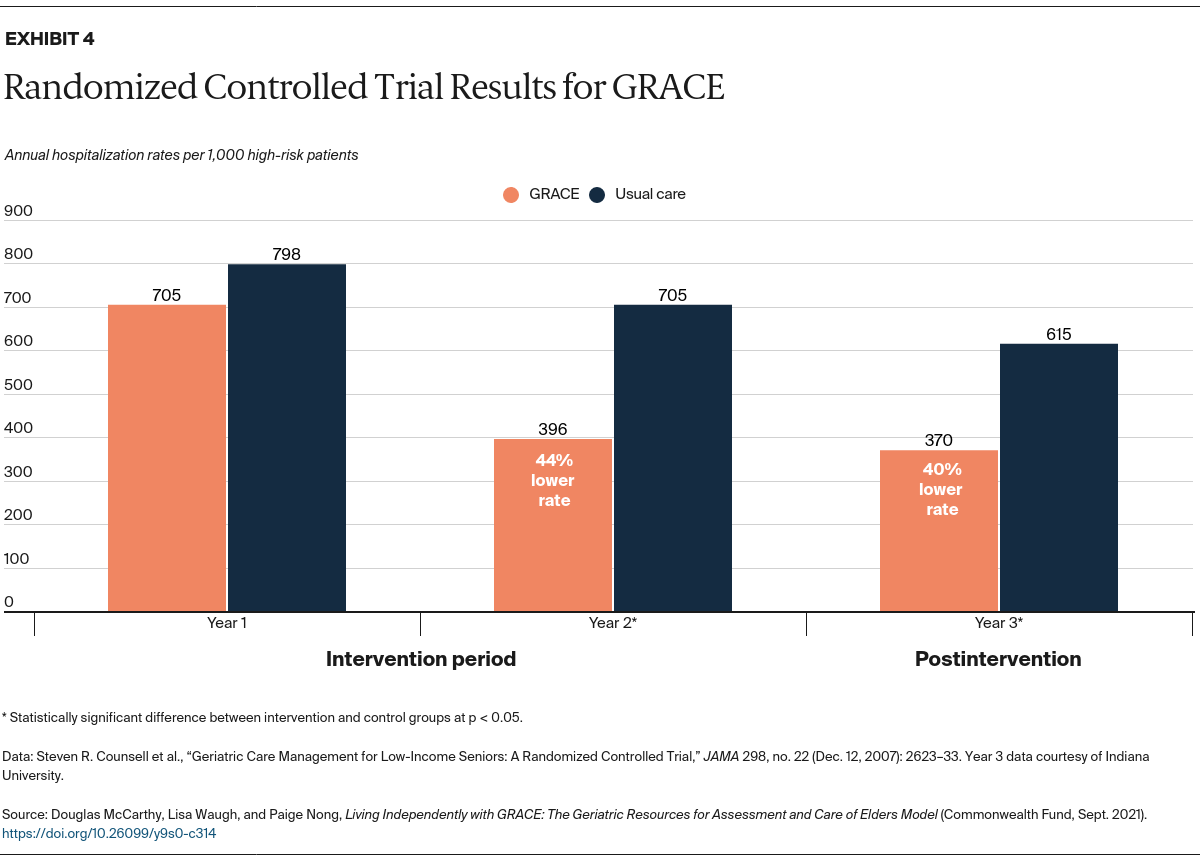
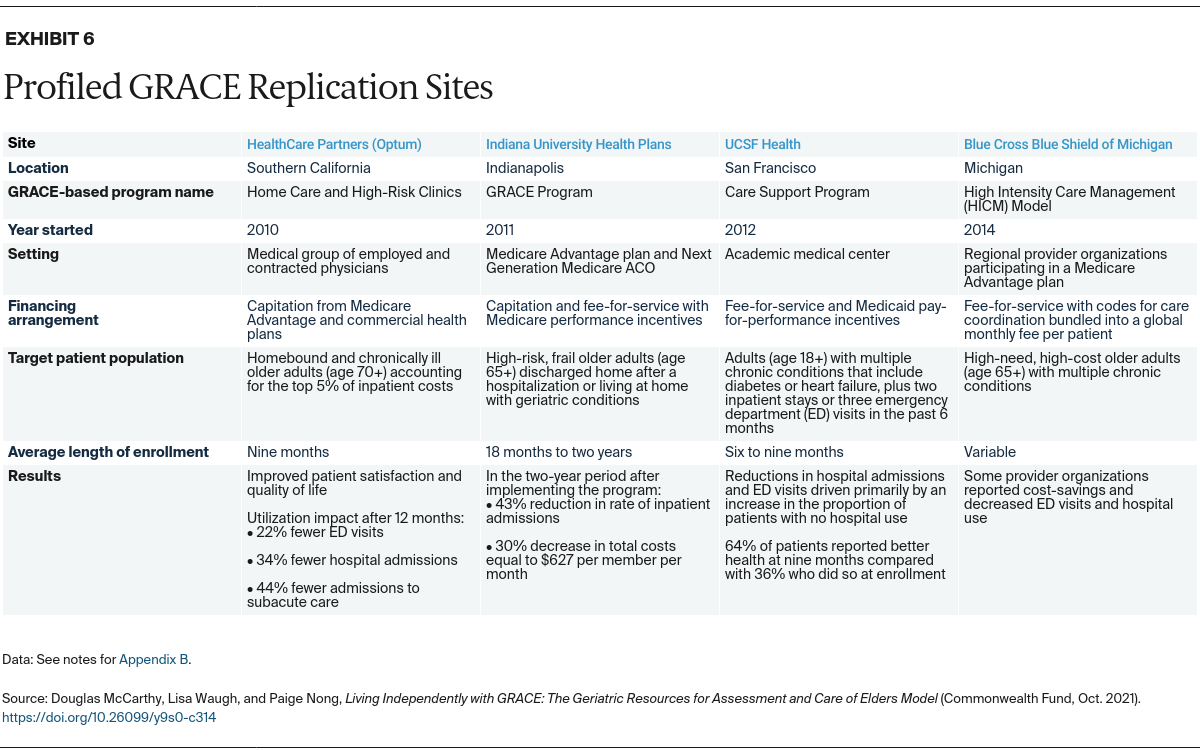
Amid a growing number of care management programs, the GRACE model stands out for its enhanced primary care, with a focus on geriatric conditions and medication management, and its integrated approach to meeting health and social needs. The care model has been proven in a controlled trial and applied in multiple sites and settings including home-based primary care, which is of growing interest because of the COVID-19 pandemic.3
This case study — one in a series describing models of care for high-need, high-cost patients — illustrates how the GRACE model has been used in diverse settings to improve care and reduce costs.
How Grace Works
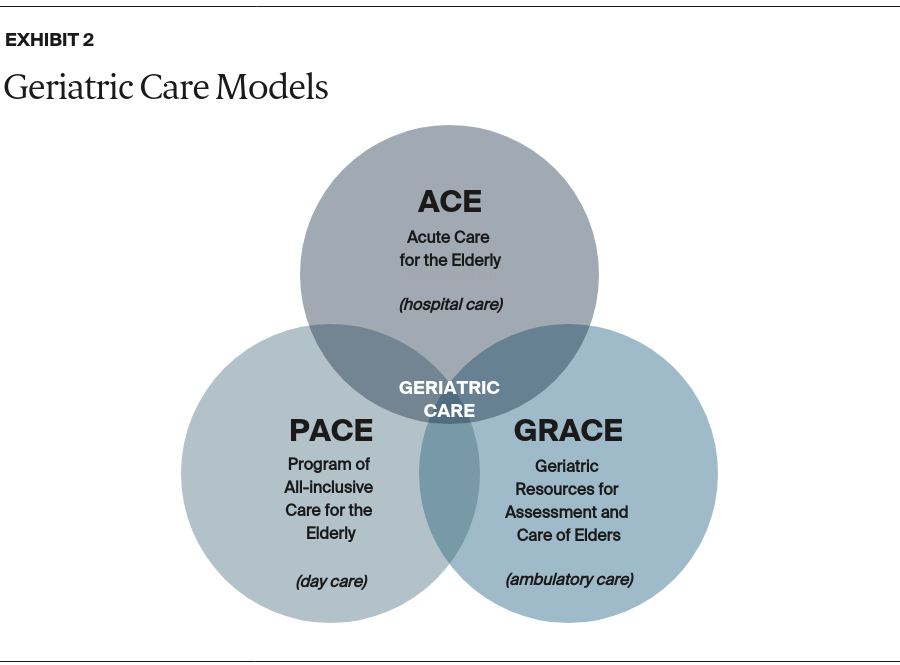
The GRACE model was inspired by other geriatric care models delivered in hospitals and day-care settings (Exhibit 2). With its focus on ambulatory care, the model allows patients to maintain relationships and continuity with their primary care providers.
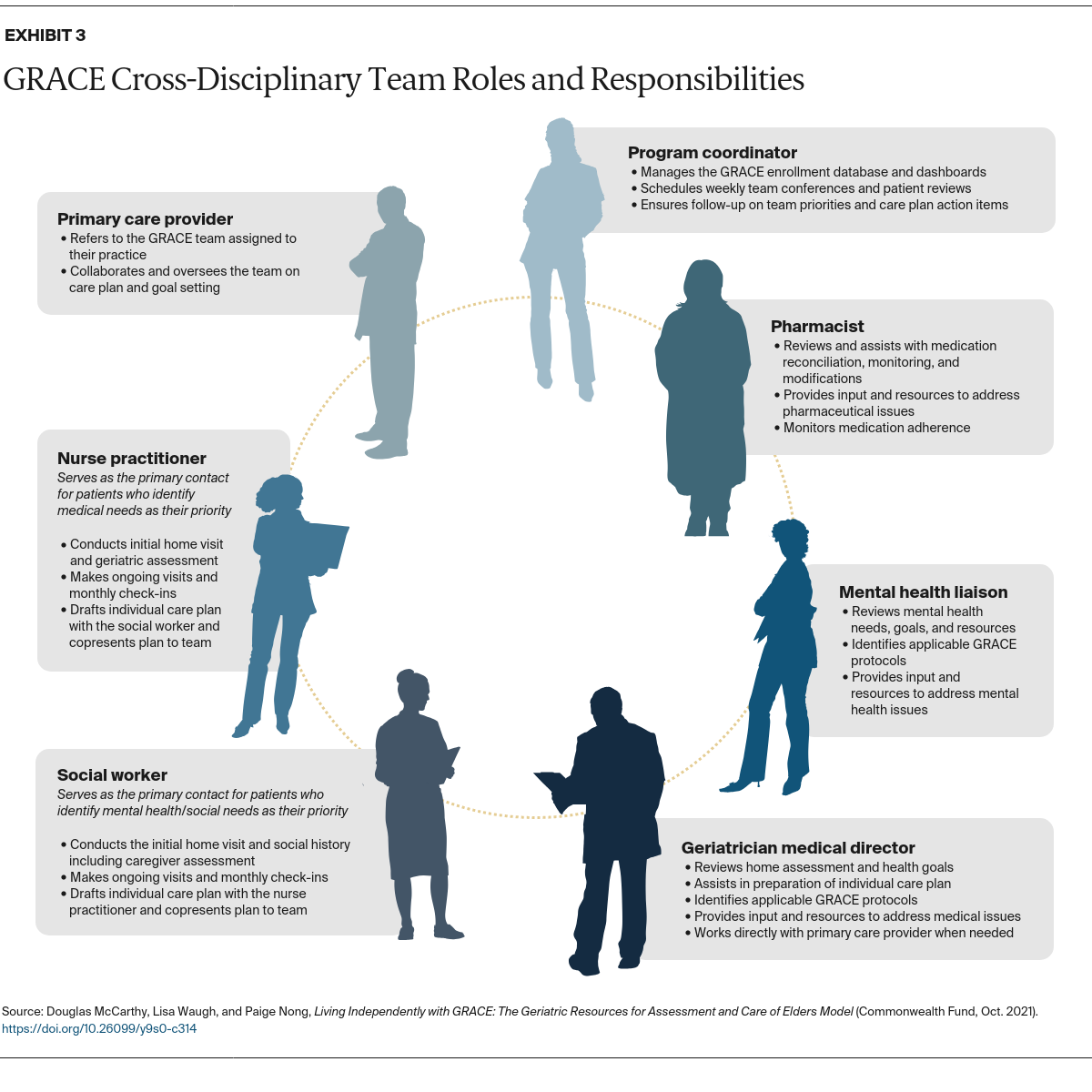
The primary goals of GRACE are to optimize the health and functional status of patients living at home while reducing their need for hospital care.4 At the heart of the model is a nurse practitioner–social worker dyad. Together, they provide care management to patients in coordination with the primary care provider and a cross-disciplinary team (Exhibit 3). The nurse practitioner–social worker dyad addresses the physical, mental, and social needs of patients with multiple chronic conditions who may have functional limitations that require the support of a caregiver. Notably, GRACE specifically addresses the geriatric needs of older patients with dementia and depression, who may not be well served by routine care management programs.