

Abstract
A new survey from The Commonwealth Fund and The Kaiser Family Foundation asked primary care providers—physicians, nurse practitioners, and physician assistants—about their experiences with and reactions to recent changes in health care delivery and payment. Providers’ views are generally positive regarding the impact of health information technology on quality of care, but they are more divided on the increased use of medical homes and accountable care organizations. Overall, providers are more negative about the increased reliance on quality metrics to assess their performance and about financial penalties. Many physicians expressed frustration with the speed and administrative burden of Medicaid and Medicare payments. An earlier brief focused on providers’ experiences under the ACA’s coverage expansions and their opinions about the law.
OVERVIEW
In recent years, the U.S. primary care delivery system has experienced many changes in the way health care is organized, delivered, and financed. Some of these changes have been strengthened or accelerated by the Affordable Care Act (ACA). For instance, there has been an increased use of health information technology, a move toward team-based care and using nonphysician clinicians, an effort to better coordinate care through medical homes and accountable care organizations, and the introduction of financial incentives and quality metrics to determine how providers are paid.
Using data from the Commonwealth Fund/Kaiser Family Foundation 2015 National Survey of Primary Care Providers, this brief examines providers’ opinions about the changes in primary care payment and health care delivery. Between January 5 and March 30, 2015, a nationally representative sample of 1,624 primary care physicians and a separate sample of 525 midlevel clinicians (i.e., nurse practitioners and physician assistants) working in primary care practices were surveyed online and by mail.
The survey finds that providers’ experiences with new models of care and changes to the health care system are varied. Slightly more than half of primary care physicians reported receiving financial incentives based on the quality or efficiency of care, although one-third of physicians continue to be paid exclusively on a fee-for-service basis. Three of 10 primary care physicians said their practice is qualified as a patient-centered medical home (PCMH) or advanced primary care practice. A similar share is currently participating in accountable care organizations (ACO). Nurse practitioners and physician assistants reported lower levels of participation in ACOs than did physicians, and many were unsure whether their practice participates in one or not.
Health information technology generally garnered positive opinions. Though seemingly counterintuitive, this finding is consistent with the literature: while providers tend to dislike transitioning from paper-based charts to electronic health record software, they generally accept the promise of HIT as a concept.1 On other trends, primary care providers’ views were divided or skewed negative. Both physicians and midlevel clinicians were more likely to say that increased use of medical homes is having a positive rather than a negative impact on the ability to provide quality care, but large shares said there has been no impact or they are not sure. Among providers working in practices that receive incentives for qualifying as medical homes, views were more positive.
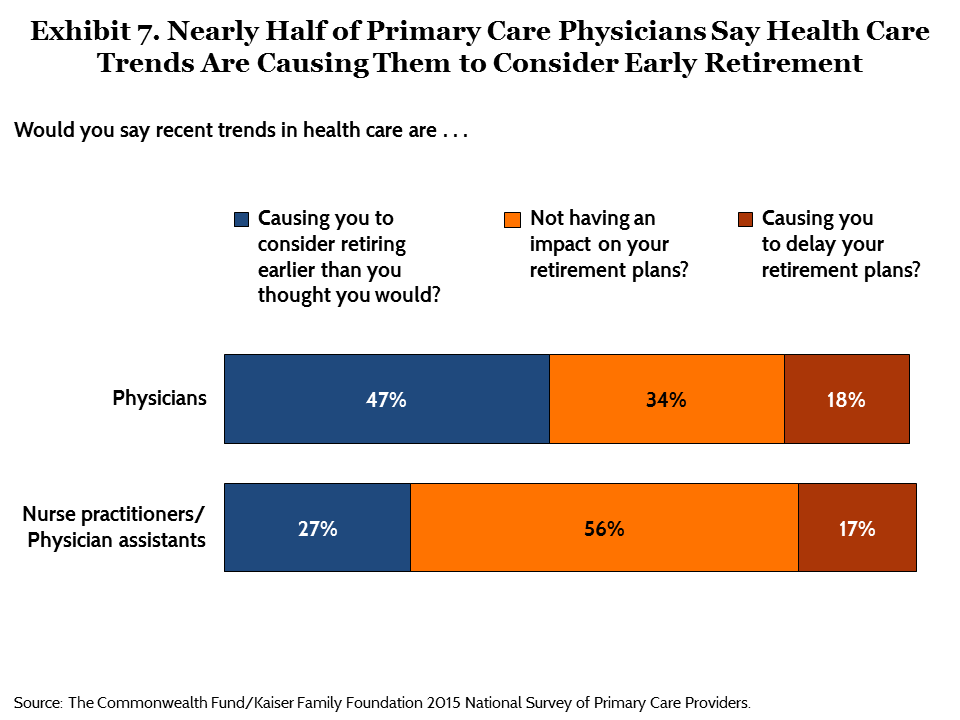
In contrast, physicians’ views tilt negative on the effect ACOs have had on the quality of care, and many are still not sure of their effect. Among physicians working in ACOs, views were divided between positive and negative. Providers were more negative about the use of quality metrics to assess their performance, even those providers who receive incentive payments based on quality. Nearly half of physicians and about a quarter of nurse practitioners and physician assistants said recent trends in health care are causing them to consider early retirement. However, a large majority of providers report satisfaction with their medical practice overall, consistent with historical data over the past two decades.2,3
SURVEY FINDINGS IN DETAIL
The Changing Primary Care Practice Environment
Current efforts to change primary care payment—that is, using new models that replace fee-for-service payment with other approaches—have been accelerated by provisions in the ACA. About two-thirds of primary care physicians (64%) reported they are paid either by capitation (i.e., prepayments for a set of services for a defined number of patients) or salary (i.e., predetermined income for an entire panel of patients) or through a combination of capitation, salary, and fee-for-service (Table 1). Nearly nine of 10 nurse practitioners and physician assistants (87%) reported receiving payment through mechanisms that are not exclusively fee-for-service. Nevertheless, about a third of primary care physicians (34%) are still paid exclusively on a fee-for-service basis. More than half (55%) of physicians and about a third (34%) of nurse practitioners and physician assistants said their practice receives incentives or payments based on measures of quality of care, patients’ experiences, or efficiency of providing care. About one-third of nurse practitioners and physician assistants were unsure whether they had received such incentives.
Table 1. Practice Characteristics
| Physicians | Nurse practitioners/ Physician assistants |
|
| Unweighted N | 1,624 | 525 |
| % | % | |
| Practice has consolidated with or been acquired by a group practice, a hospital, or another type of organization in the past two years |
17 | 16 |
| How are you paid for seeing patients? | ||
| Fee-for-service only | 34 | 10 |
| Capitation or salary, with/without fee-for-service | 64 | 87 |
| Provider or practice is currently receiving incentives or payments based on the following: |
||
| Quality of care or patient experiences | 50 | 27 |
| Utilization or efficiency in care | 43 | 27 |
| Either quality/patient experiences or utilization/efficiency (NET) | 55 | 34 |
| Qualifying as a patient-centered medical home (PCMH) or advanced primary care practice (APCP) |
30 | 26 |
| Is your practice currently participating or preparing to participate in an ACO arrangement with Medicare or private insurers? |
||
| Yes, currently participating | 29 | 18 |
| Yes, preparing to participate | 9 | 6 |
| No | 32 | 19 |
| Not sure | 28 | 56 |
| Number of providers accepting Medicare | N=1,217 | N=377 |
| Among these, percent currently participating in ACOs | 34 | 22 |
Source: The Commonwealth Fund/Kaiser Family Foundation 2015 National Survey of Primary Care Providers.
Several newer models of delivering care, such as the patient-centered medical home (or PCMH, a model of care that emphasizes comprehensive care coordination, care teams, patient engagement, and population care management) and the accountable care organization (or ACO, a model in which several types of health care providers collectively take responsibility for the quality and costs of care for a population of patients), specifically aim to improve the way care is organized, paid for, and delivered. Twenty-nine percent of all primary care physicians said they participate in an ACO arrangement with Medicare or private insurers; 34 percent of those who accept Medicare also said they participate (Table 1). Similarly, about 30 percent of physicians reported receiving incentives or payments for qualifying as a PCMH or through the ACA’s Advanced Primary Care Practice (APCP) medical home demonstration.4 Fewer than two of 10 (18%) nurse practitioners and physician assistants reported currently participating in an ACO, and about one-quarter (26%) said their practices qualified as a patient-centered medical home or an advanced primary care practice. A substantial percentage of providers (28% of physicians and 56% of nurse practitioners and physician assistants) are unsure whether their practices participate in ACO arrangements.
Another recent trend is the consolidation and acquisition of physician practices. The survey finds that about one of six providers (17% of physicians and 16% of nurse practitioners and physician assistants) reported their practices were acquired by or consolidated with a group practice, hospital, or another type of organization within the past two years (Table 1).
Mixed Views of New Models and Tools
The survey asked primary care providers what effect, if any, they think these new models are having on providers’ ability to provide high-quality care to patients. Health information technology received the most positive ratings, with half (50%) of physicians and nearly two-thirds (64%) of nurse practitioners and physician assistants saying it has made a positive impact (Table 2).
Table 2. Providers' Opinions About the Impact of Health Information Technology and
Financial Penalties for Unnecessary Hospital Admissions on Quality of Care for Patients
| Physicians | Nurse practitioners/ Physician assistants |
|
| Unweighted N | 1,624 | 525 |
| % | % | |
| Do you think each of the following is having a positive, negative, or no impact on primary care providers' ability to provide quality care to their patients? | ||
| Increased use of health information technology | ||
| Positive impact | 50 | 64 |
| Negative impact | 28 | 20 |
| No impact | 10 | 8 |
| Not sure | 11 | 7 |
| Increased use of programs that include financial penalties for unnecessary hospital admissions or readmissions | ||
| Positive | 12 | 15 |
| Negative | 52 | 41 |
| No impact | 14 | 11 |
| Not sure | 21 | 32 |
Source: The Commonwealth Fund/Kaiser Family Foundation 2015 National Survey of Primary Care Providers.
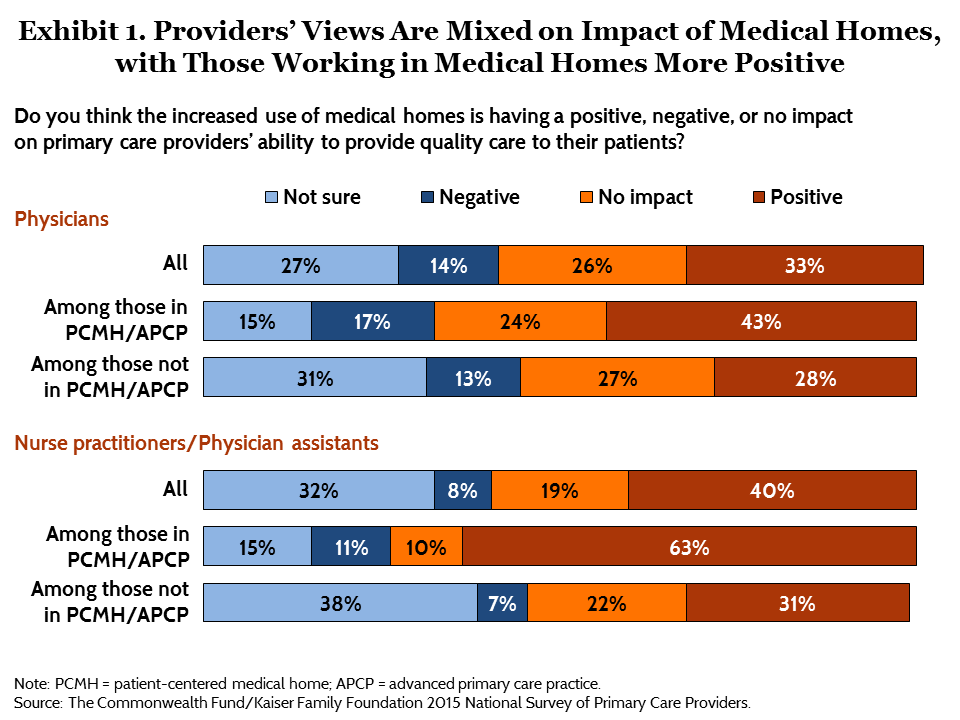
Views were more mixed about medical homes and ACOs. Overall, one-third (33%) of physicians and four of 10 (40%) nurse practitioners and physician assistants said they believe medical homes are having a positive impact on quality of care (Exhibit 1), while roughly one of 10 said the impact has been negative. About a quarter of each group said there has been no impact or they are not sure. Among those in practices currently receiving incentives or payments for qualifying as a PCMH or APCP, larger percentages expressed positive views of the impact of medical homes (43% of physicians and 63% of nurse practitioners and physician assistants).
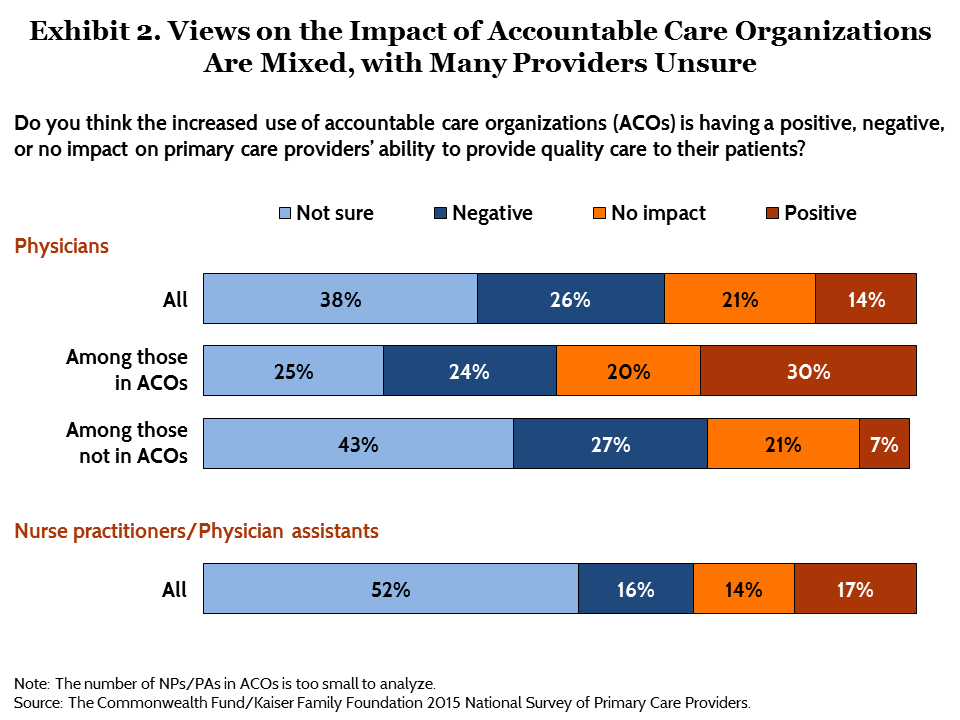
The potential of ACO arrangements to enhance quality of care also garnered mixed reviews, with large shares of providers unsure or negative about their impact. Physicians were more likely to view the increased prevalence of ACOs as having a negative (26%) rather than positive (14%) impact on quality of care, while nurse practitioners and physician assistants were more evenly split (Exhibit 2). Nearly four of 10 physicians (38%) and more than half of nurse practitioners and physician assistants (52%) were not sure of ACOs’ effect on the quality of care provided to the nearly 24 million patients enrolled in them.5 Among the 29 percent of physicians currently participating in an ACO, three of 10 said ACOs are having a positive impact, one-quarter said their impact is negative, and 20 percent said they have no impact. Even among physicians who participate in ACOs, one of four are still unsure of their impact.
Quality Metrics and Financial Penalties Are Unpopular with Providers
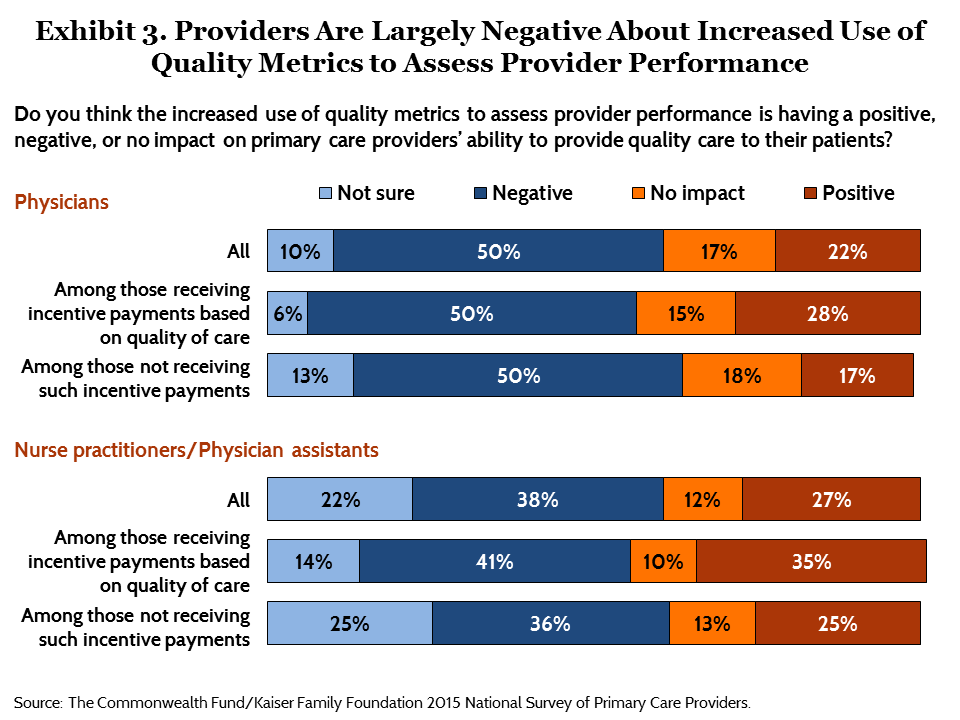
Perhaps unsurprisingly, the survey finds that performance assessments and financial penalties tied to patients’ outcomes are unpopular among providers. Half of physicians (50%) and nearly four of 10 nurse practitioners and physician assistants (38%) feel that the increased use of quality metrics to assess provider performance is having a negative impact on quality of care. Far fewer providers (22% of physicians, 27% of nurse practitioners and physician assistants) perceived a positive effect (Exhibit 3). Positive views were only slightly higher among those providers who reported receiving quality-of-care-based incentives.
Similarly, fewer than one of six primary care providers (12% of physicians, 15% of nurse practitioners and physician assistants) said that programs that include financial penalties for unnecessary hospital admissions or readmissions have a positive effect on quality of care (Table 2). Far more providers—52 percent of physicians and 41 percent of nurse practitioners and physician assistants—think these financial penalties are having a negative effect.
Views of Team-Based Care Differ Among Physicians vs. Nurse Practitioners and Physician Assistants
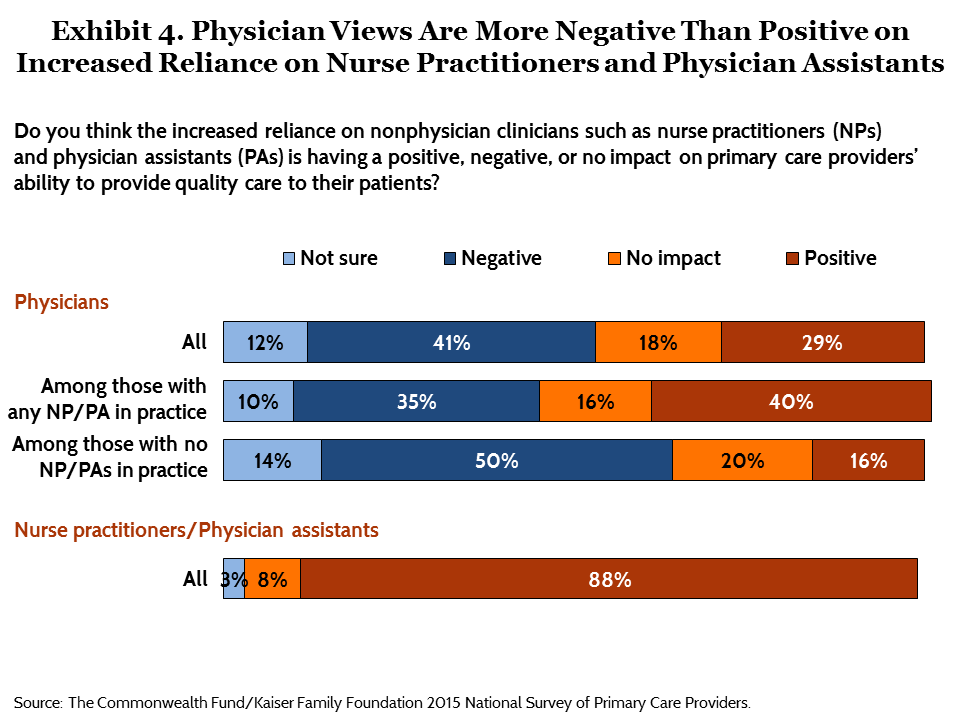
Many of the emerging models and tools to improve care delivery involve reorganization of staff roles, a shift to team-based care, and a greater reliance on nonphysicians.6 Physicians have very different views from nurse practitioners and physician assistants about the use of nonphysician clinicians in primary care. Nearly nine of 10 (88%) nurse practitioners and physician assistants viewed this change positively, while only about one of three physicians (29%) agreed (Exhibit 4). Four of 10 physicians overall (41%) said this shift is negatively affecting providers’ ability to provide quality care, but physicians’ views largely depend on whether they have a nurse practitioner or physician assistant in their practice. Among physicians with any nurse practitioner or physician assistant staff, 40 percent reported a positive view of this trend and 35 percent reported a negative view.
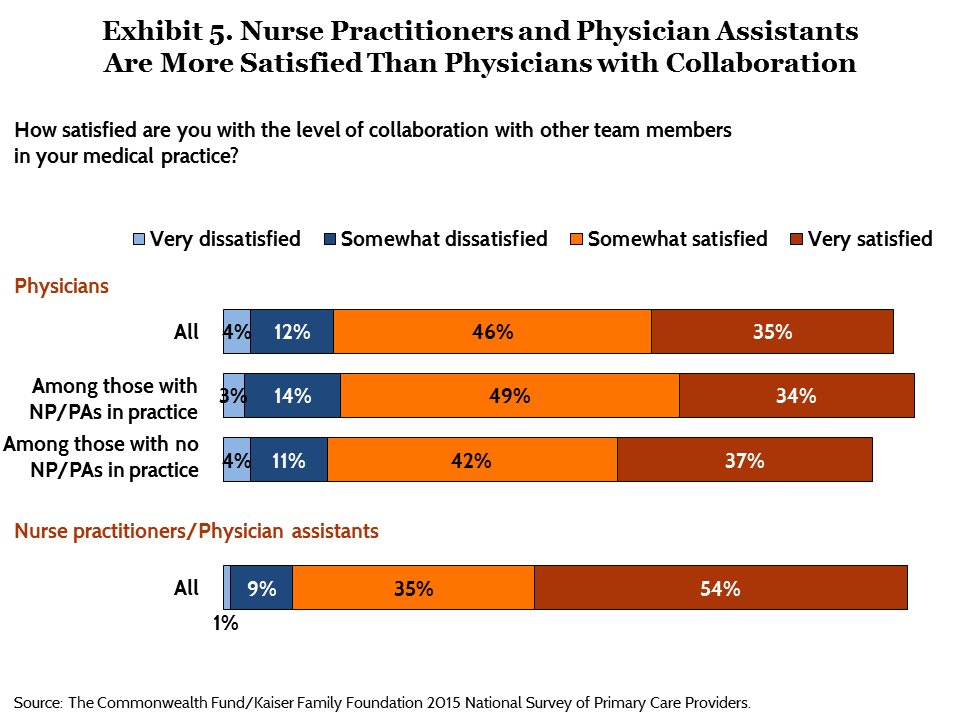
The survey also asked providers about teamwork and collaboration. When providers were asked whether they were satisfied with the level of collaboration with other team members in their practice, most said they were either somewhat or very satisfied (81% of physicians, 89% of nurse practitioners and physician assistants). However, more nurse practitioners and physician assistants than physicians said they were very satisfied (Exhibit 5). Physicians with any nurse practitioners or physician assistants in their practice (83%) and those without (79%) were generally satisfied with the level of collaboration in their practices.
Providers Rate Private Insurers More Positively Than Public Insurers
The survey asked providers to rate Medicaid, Medicare, and private insurers in terms of their reimbursement rates and administrative burden. On the whole, fewer than half of physicians gave positive ratings to any type of insurer on measures related to reimbursement, though ratings were higher for private insurers and lowest for Medicaid, with Medicare falling in the middle. Nearly half of physicians (46%) accepting private insurance considered these insurers’ payment rates to be good or excellent, with far fewer physicians—only 11 percent—rating Medicaid as highly (Exhibit 6). Medicare ranked in the middle, with 21 percent of physicians who accept it for payment stating that payment rates are good or excellent.
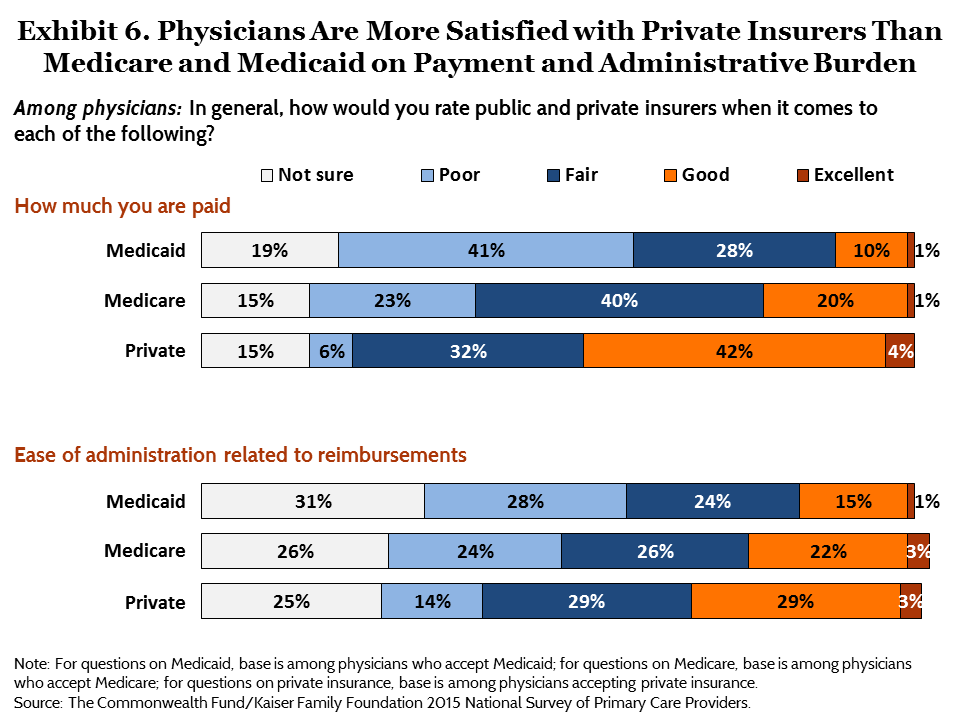
Only 16 percent of physicians accepting Medicaid rated ease of reimbursement as good or excellent. Twice as many physicians accepting private insurance rated private insurers this highly (32%). Again, Medicare falls in the middle, with 25 percent of physicians rating ease of reimbursement as good or excellent. Across the board, providers do not think Medicaid performs as well as either private insurance or Medicare in payment and administration. However, a substantial share of physicians said they were unable to assess any of these payers’ performance. Nurse practitioners and physician assistants may be even more insulated from reimbursement issues and thus more apt to say they are unsure about insurers’ payment practices (data not shown).
Nearly Half of Physicians Say Trends Are Leading Them to Consider Early Retirement
Nearly half (47%) of physicians and about a quarter (27%) of nurse practitioners and physician assistants said that recent trends in health care are causing them to consider retiring earlier than they originally thought they would (Exhibit 7). While physician dissatisfaction is associated with early retirement, a look at historical trends shows that physician satisfaction levels have not changed dramatically over the past 20 years.7 About one of six in each group said that trends are making them consider delaying their retirement (18% of physicians and 17% of nurse practitioners and physician assistants), while a third (34%) of physicians and more than half (56%) of nurse practitioners and physician assistants said these trends are not having much impact on their retirement plans.
CONCLUSION
New primary care payment and delivery models have emerged in recent years as part of efforts to improve patient outcomes and lower health care costs, with the Affordable Care Act accelerating many of these changes. It may be too early to reach a conclusion on the quality or cost effects of these primary care reforms, but assessing the perspective and experience of those on the front lines is critical to understanding the implementation of these reforms, including any challenges that could potentially undermine the process.
The survey results indicate that primary care providers’ views of many of these new models are more negative than positive. There are exceptions: health information technology gets mostly positive views and medical homes receive mixed opinions with a positive tilt. With regard to HIT, our study indicates that primary care providers generally accept the promise of HIT to improve quality of care even if previous research shows they dislike the process of transitioning from paper-based records.8 Our survey results also may reflect clinicians’ earlier exposure to certain models and tools. National adoption of electronic health records received a boost from the Health Information Technology for Economic and Clinical Health (HITECH) Act of the federal stimulus package of 2009, while the four primary care specialty societies announced a joint statement regarding medical homes in February 2007, several years before passage of the Affordable Care Act.
Though many providers are unsure of the impact of ACOs on quality of care, those physicians who do have an opinion are more likely to say ACOs are a having a negative rather than a positive impact on quality of care. ACO implementation is a somewhat more recent development, and primary care providers are not as involved in the day-to-day management of organizational change. Primary care clinicians’ views are also decidedly negative when it comes to financial penalties and the increased use of quality metrics in judging their performance. It may be some time before they can become comfortable with these new payment models.
More primary care providers may be participating in ACOs and relying on quality metrics for performance assessment in the near future. In early 2015, the Centers for Medicare and Medicaid Services announced that 85 percent of Medicare fee-for-service payments should be tied to quality or value by 2016. And, by the end of 2018, 50 percent of all Medicare payments should be tied to quality or value through specific alternative payment models, like ACOs and bundled payments.9 Dissatisfaction with new models may not be solely attributable to a difficult transformation process; larger culture change within the practice of medicine may be a necessary first step before delivery system reforms such as ACOs and medical homes are fully accepted on the ground.
As primary care transformation efforts mature and spread, it will remain important to judge their effects on patients in terms of access, quality, and costs of care. However, it is also important to assess their effect on primary care clinicians. Of concern, nearly half of primary care physicians say that recent trends in health care are causing them to consider retiring earlier than planned. Market trends in health care have been affecting physicians’ satisfaction for more than 20 years. It will be important to monitor providers’ satisfaction with delivery reform efforts.
| Contributors to this brief include Jamie Ryan, Michelle Doty, Liz Hamel, Mira Norton, Melinda Abrams, and Mollyann Brodie. |
MethodologyThe Commonwealth Fund/Kaiser Family Foundation 2015 National Survey of Primary Care Providers was jointly designed and analyzed by researchers at The Commonwealth Fund and The Kaiser Family Foundation (KFF). Social Science Research Solutions (SSRS) carried out the field work and collaborated with Commonwealth Fund and Kaiser researchers on questionnaire design, pretesting, sample design, and weighting. The Commonwealth Fund and The Kaiser Family Foundation each contributed financing for the survey. The project team included Jamie Ryan, Michelle Doty, Rose Kleiman, and Melinda Abrams from The Commonwealth Fund; and Liz Hamel, Mira Norton, and Mollyann Brodie from Kaiser. Survey responses were collected via hard copy and Web-based questionnaires between January 5 and March 30, 2015, with a random sample of 1,624 primary care physicians and a separate random sample of 366 nurse practitioners (NPs) and 159 physician assistants (PAs) working in primary care practices. The surveys achieved the following response rates, calculated using AAPOR’s RR3: physicians (34%), NPs (29%), and PAs (25%). The sample for physicians was procured from SK&A, which maintains a national database of physicians that is continuously updated by a telephone verification process. Physicians drawn for the sample were those whose specialty was listed in the SK&A database as either general practice, family practice, internal medicine, adolescent medicine, internal medicine pediatrics, general pediatrics, or geriatrics. Physicians were further screened to include only those who indicated in the survey that they spend at least 60 percent of their work time providing care to patients as a primary care provider. The physician sample included an oversample of physicians working in low-income areas (those whose office is located in a zip code where the average annual household income is $55,000 or less) and those working in federally qualified health centers and community health centers. The sample for NPs/PAs was procured from KM Lists, which uses publicly released data available from state licensing boards and information from professional associations and journal subscriptions to develop and update its database. Unlike physicians, specialty type for NPs and PAs does not necessarily correspond with the practice setting in which they work. Therefore, a broader list of specialties was included. NPs and PAs drawn for the sample were those whose specialty was listed in the database as family medicine, internal medicine, adult medicine, adolescent medicine, pediatrics, internal medicine pediatrics, geriatrics, preventive medicine, osteopathy, women’s health, or community/public health. The sample also included NPs and PAs whose specialty type was listed as “unknown” (these were undersampled relative to the other listed specialties). NPs and PAs were further screened to include only those who indicated in the survey that they are currently working in a primary care practice and that they spend at least 60 percent of their work time providing care to patients as a primary care provider. In an effort to maximize contact and completion rates, providers were contacted by multiple modes (mail, telephone, and email), offered incentives, and given the option of completing the survey in hard copy or online. A multistage weighting process was applied to ensure an accurate representation of the national population of primary care physicians and NPs/PAs. The first stage in weighting both samples involved corrections for sample design and differential nonresponse by email availability. Physician survey data were weighted by gender, age, specialty type, region, and site specialty using benchmarks in the 2014 American Medical Association Physicians Masterfile; and number of MDs at site using benchmarks in the SK&A list of primary care MDs. NP and PA data were weighted by gender and specialty type using benchmarks in the KM Lists. The physician sample was analyzed separately from the NP and PA sample. All statistical tests of significance account for the effect of weighting. The margin of sampling error (MOSE) including the design effect is plus or minus 3 percentage points for MDs and 5 percentage points for the combined group of NPs and PAs. Unweighted Ns and MOSE for NPs and PAs separately are shown in the table below. For results based on other subgroups, the MOSE may be higher.
|
Notes
1 M. W. Friedberg, P. G. Chen, K. R. Van Busum et al., Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy (Santa Monica, Calif.: RAND Corporation, 2013).
2 The Kaiser Family Foundation and The Commonwealth Fund, Experiences and Attitudes of Primary Care Providers Under the First Year of ACA Coverage Expansion—Findings from the Kaiser Family Foundation/Commonwealth Fund 2015 National Survey of Primary Care Providers (Menlo Park, Calif., and New York: The Henry J. Kaiser Family Foundation and The Commonwealth Fund, June 2015).
3 B. E. Landon, J. Reschovsky, and D. Blumenthal, “Changes in Career Satisfaction Among Primary Care and Specialist Physicians, 1997–2001,” Journal of the American Medical Association, Jan. 22–29, 2003 289(4):442–49.
4 FQHC Advanced Primary Care Practice Demonstration, http://innovation.cms.gov/initiatives/fqhcs/.
5 D. Muhlestein, “Growth and Dispersion of Accountable Care Organizations in 2015,” Health Affairs Blog, March 31, 2015, http://healthaffairs.org/blog/2015/03/31/growth-and-dispersion-of-accountable-care-organizations-in-2015-2/.
6 E. H. Wagner, K. Coleman, R. J. Reid et al., “The Changes Involved in Patient-Centered Medical Home Transformation,” Primary Care: Clinics in Office Practice, June 2012 39(2):241–59.
7 B. E. Landon, J. D. Reschovsky, H. H. Pham et al., “The Consequences of Physician Dissatisfaction,” Medical Care, March 2006 44(3):234–42; Landon, Reschovsky, and Blumenthal, “Changes in Career Satisfaction,” 2003.
8 Friedberg, Chen, Van Busum et al., Factors Affecting Physician Professional Satisfaction, 2013.
9 S. M. Burwell, “Setting Value-Based Payment Goals—HHS Efforts to Improve U.S. Health Care,” New England Journal of Medicine, March 5, 2015 372(10):897–99.
