Abstract
- Issue: Older Americans who need help with daily activities, such as bathing or managing medications, most often live in the community with the support of family and other unpaid caregivers. Little is understood about the adverse consequences this population suffers when no one is available to help with task-specific needs.
- Goal: To assess the prevalence of adverse consequences due to unmet long-term services and supports (LTSS) needs. To identify whether and how caregiving characteristics are associated with adverse consequences and whether such factors differ among older adults with and without dementia.
- Methods: We analyzed the 2017 National Health and Aging Trends Study (NHATS) and National Study of Caregiving (NSOC).
- Key Findings: More than four in 10 community-living older adults experienced adverse consequences due to unmet LTSS needs. Older adults with dementia, greater LTSS needs, and low incomes were more likely to experience adverse consequences. Other factors associated with a higher likelihood of adverse consequences included the number of caregivers helping an older adult.
- Conclusions: Policies that account for the complexity of care needs among older adults living in the community with disability and better support for family and unpaid caregivers could help prevent adverse consequences.
Introduction
Most older Americans with disabilities live in the community — outside of nursing homes and residential care facilities — and receive long-term services and supports (LTSS) to assist with their daily activities, such as bathing, dressing, and meal preparation.1 For the majority of those with LTSS needs, family and other unpaid caregivers are the ones providing this help.
But Medicare does not cover LTSS beyond home health services in limited circumstances. Moreover, most older adults are not eligible for Medicaid-funded Home and Community-Based Services; those who are eligible often are placed on waiting lists for extended periods.
Among older adults with LTSS needs, the adequacy of LTSS has a profound effect on quality of life, quality of care, and services used. For example, lack of mobility assistance might mean not being unable to leave one’s home. Insufficient help with toileting could mean remaining in wet or soiled clothing or missing doses of prescribed medication. These experiences can result in falls, emergency department visits, and hospitalizations.2
Prior studies have found adverse consequences due to unmet LTSS needs are more common among older adults with greater levels of disability, those enrolled in Medicaid, and those living with dementia.3 Additionally, although a caregiver’s characteristics and circumstances might affect an older adult’s experience of unmet LTSS needs,4 it is not clear to what extent such factors differ among older adults with dementia in the community.
In this issue brief, we draw on the 2017 National Health and Aging Trends Study and linked National Study of Caregiving to update understanding of the LTSS needs among noninstitutionalized older adults and their caregiving arrangements. We also provide new insights into the caregiving circumstances and experiences of older adults with dementia, a topic relevant to policy dialogue regarding the prioritization of care-based supportive policies and practices.
Findings
Adverse Consequences Due to Unmet LTSS Needs
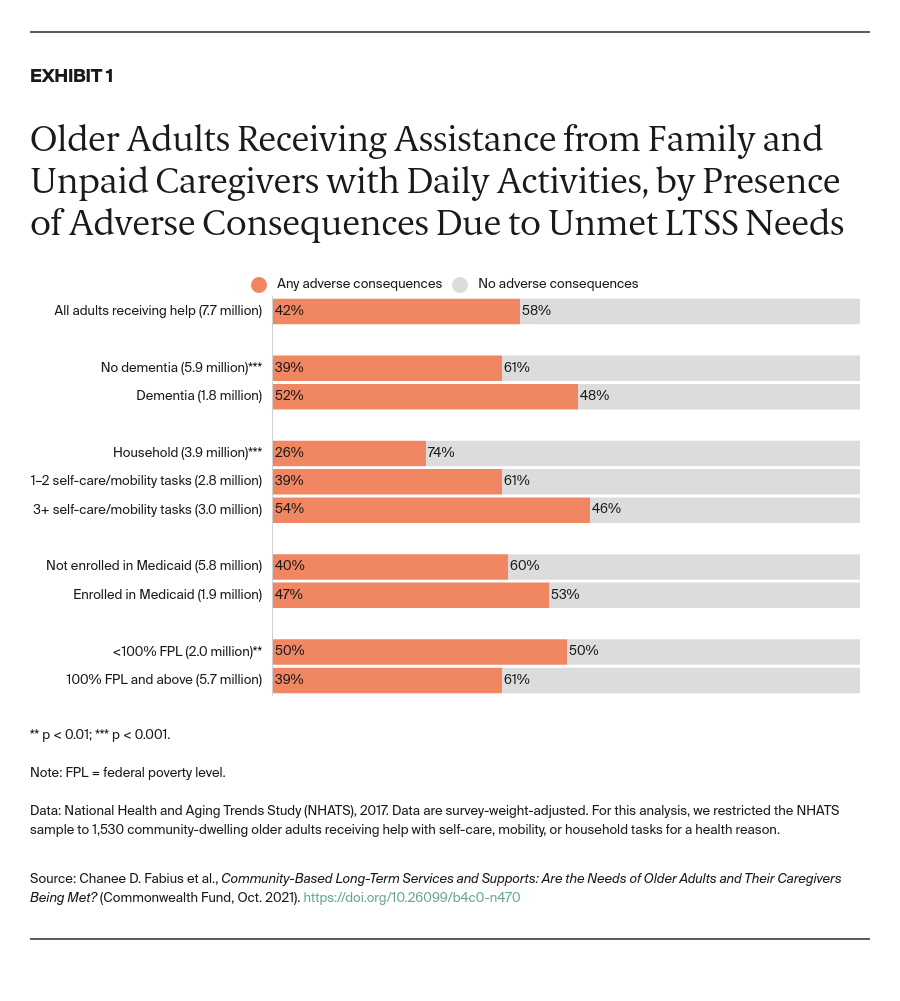
In the United States, 7.7 million community-living older adults received help from family and unpaid caregivers for health and functioning reasons in 2017. Two in five (42%) of these older adults were found to have experienced at least one adverse consequence due to unmet LTSS needs (Exhibit 1). Adverse consequences were most prevalent among those in worse health.
More than half of older adults living with dementia or receiving help with three or more self-care or mobility activities reported they experienced one or more adverse consequence. Living in poverty was also associated with a higher likelihood of adverse consequences.