The United Kingdom’s National Health Service (NHS) is the world’s first health care system to commit to achieving net-zero carbon emissions. Here we examine the history and status of the NHS efforts and identify lessons for the U.S. health care system. As the former Director of Strategy for the NHS in England, the lead author helped develop the NHS’s net-zero plan and create the Greener NHS program that is now delivering on the plan’s commitments.
Introduction
The impact of climate change on health and the contribution of health care systems to climate change have been well documented. Intensifying weather events have already resulted in the deaths of millions of people worldwide and thousands of people in the United States alone. Increasing costs, growing inequities in already at-risk communities, and declining quality due to hospital overcrowding and disruptions to the medical supply chain are the dire realities of a health care system impacted by climate change.1 Globally, the health care sector itself is responsible for as much as 4.6 percent of total greenhouse gas emissions — carbon dioxide, methane, and ozone, among others. In the United States, the share is 8.5 percent.2
Health systems around the world are taking note of these crises and beginning to respond. In 2021, as part of the United Nations Climate Change Conference (COP26), 60 countries, including the United States, committed to creating climate-resilient, low-carbon, sustainable health systems, with 20 countries committing to net-zero health care system emissions by 2050.3 Health systems that adopt a net-zero approach focus on removing carbon as quickly as possible, only as a last resort turning to mechanisms that “offset” remaining emissions that can’t be removed through other means.
The NHS was the world’s first health care system to commit to net-zero carbon emissions.4 Like many health systems around the world, the NHS is responsible for large portions of the nation’s overall carbon emissions (4%) and public-sector emissions (40%).5 As global recognition of climate change as a health emergency has grown, the NHS launched its Greener NHS program to review NHS progress to date and develop a delivery plan for getting to net zero.6 That plan, released in October 2020, offers a roadmap of actions the NHS is already taking and will take to cut its emissions.7 It established two target dates for achieving net-zero emissions: by 2040 for emissions the NHS controls directly, and by 2045 for wider emissions it only influences.
The United States has set targets to lower carbon emissions for certain health-related government facilities (like Indian Health Service facilities and Veterans Affairs hospitals), and general government service buildings are set to achieve net-zero emissions by 2045. But there is still much the U.S. health system could learn from the NHS.8 In this brief, we describe how the NHS developed and began implementing its net-zero plan and what the U.S. health system could learn as it seeks to mitigate the impact of climate change and reduce its own carbon footprint.
Developing the NHS Net-Zero Plan
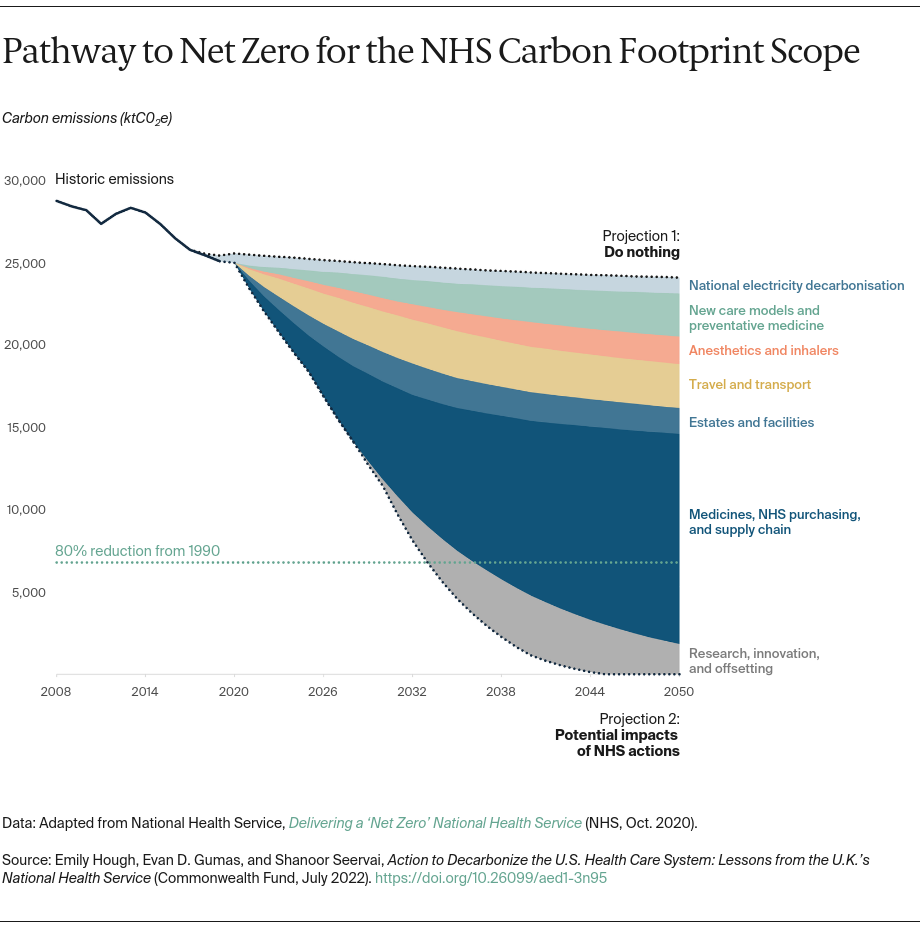
As a first step, the NHS sought to determine its total greenhouse gas emissions since 1990.9 To do this, analysts gathered calculations of carbon emissions across NHS’s major areas of emissions, including the supply chain, staff and patient travel and transport, building and energy use, and high-emitting drugs used in anesthetics and inhalers. NHS analysts projected future carbon emissions in a “no change” scenario based on recent trends in health care and transport use, as well as U.K. government forecasts.
Next, in 2020, NHS England launched a global call for evidence-based policies and actions that can reduce health care emissions. The Greener NHS team reviewed these initiatives based on their potential impact and their deliverability within the NHS, with input from a panel of experts across the fields of health care and climate change. Selected interventions were modeled against a “no change” scenario to determine their impact on future emissions and remaining gaps.
The analytical method used to develop NHS’s carbon footprint was published in 2021 to support other global health systems seeking to map their own emissions.10