Abstract
- Issue: Given shifting home health use during the COVID-19 pandemic, studying the characteristics of Medicare home health beneficiaries with respect to race and caregiver assistance may inform efforts to address disparities in access and service use.
- Goal: To identify changes in race and acuity of home health beneficiaries between 2019 and 2020, as well as access to caregiver assistance and outcomes during home health.
- Methods: Analysis of files containing 100 percent of Medicare claims for 2019 and 2020, plus a sample of Outcome and Assessment Information Set (OASIS) assessments.
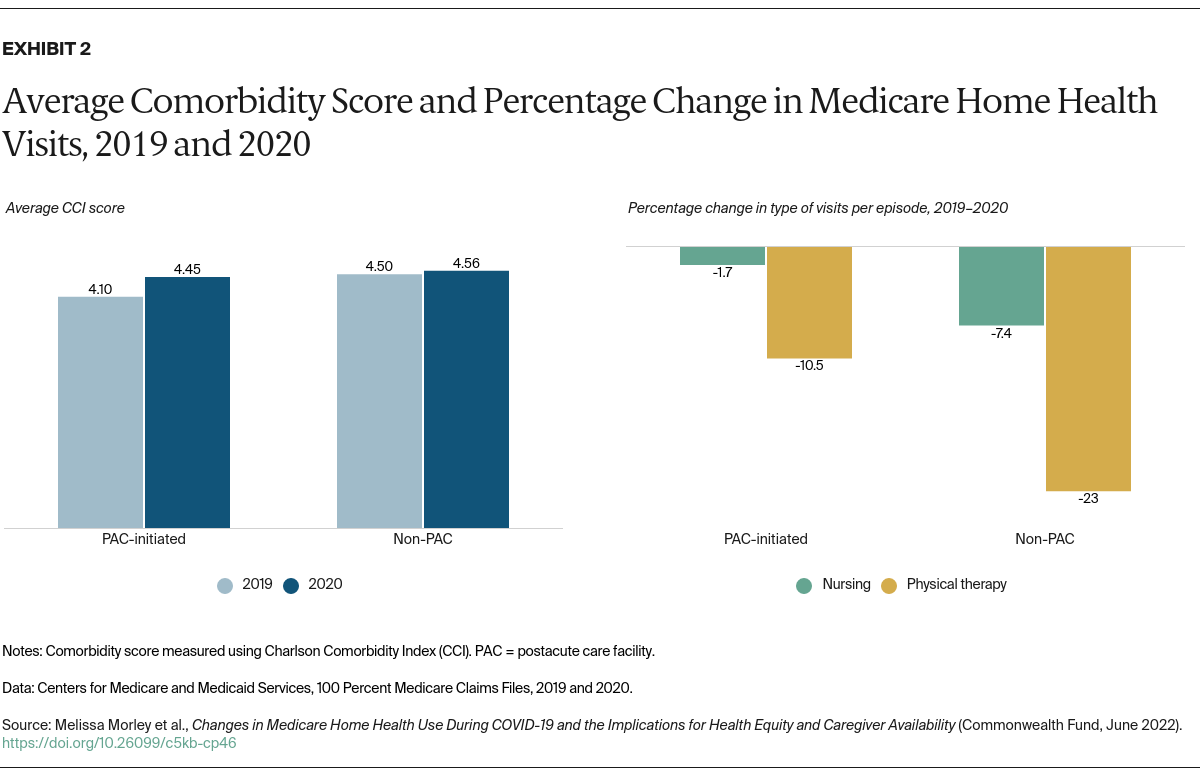
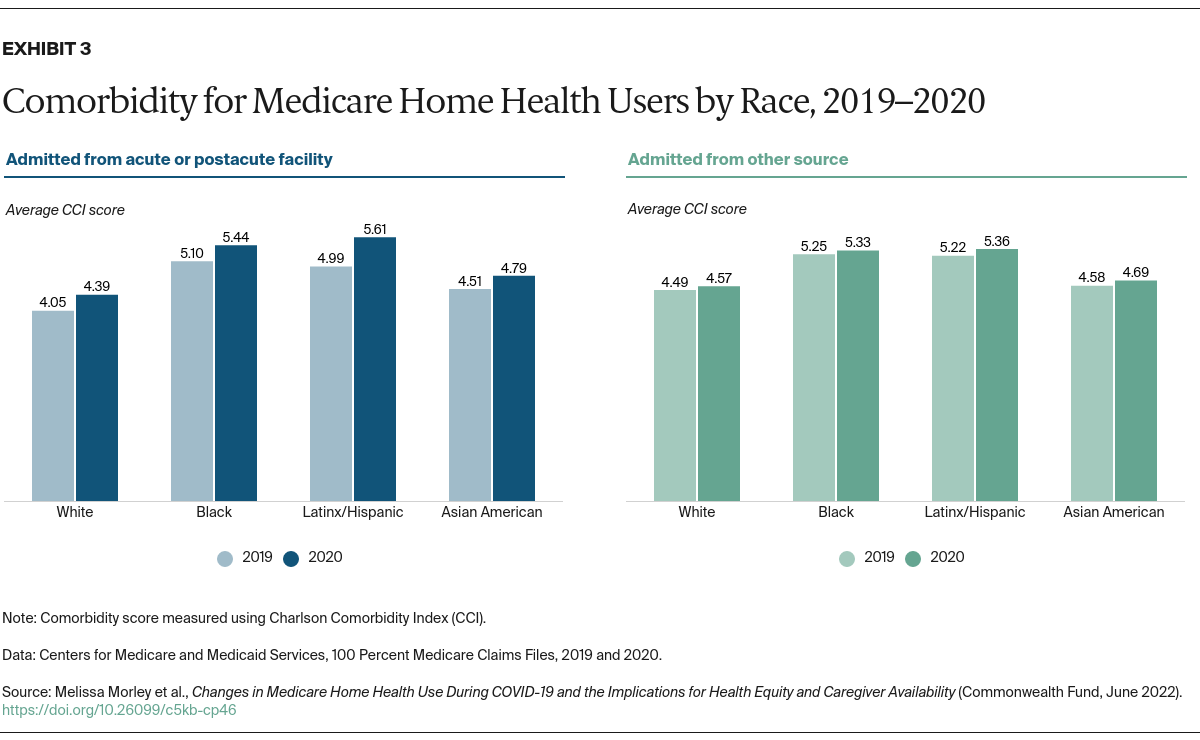
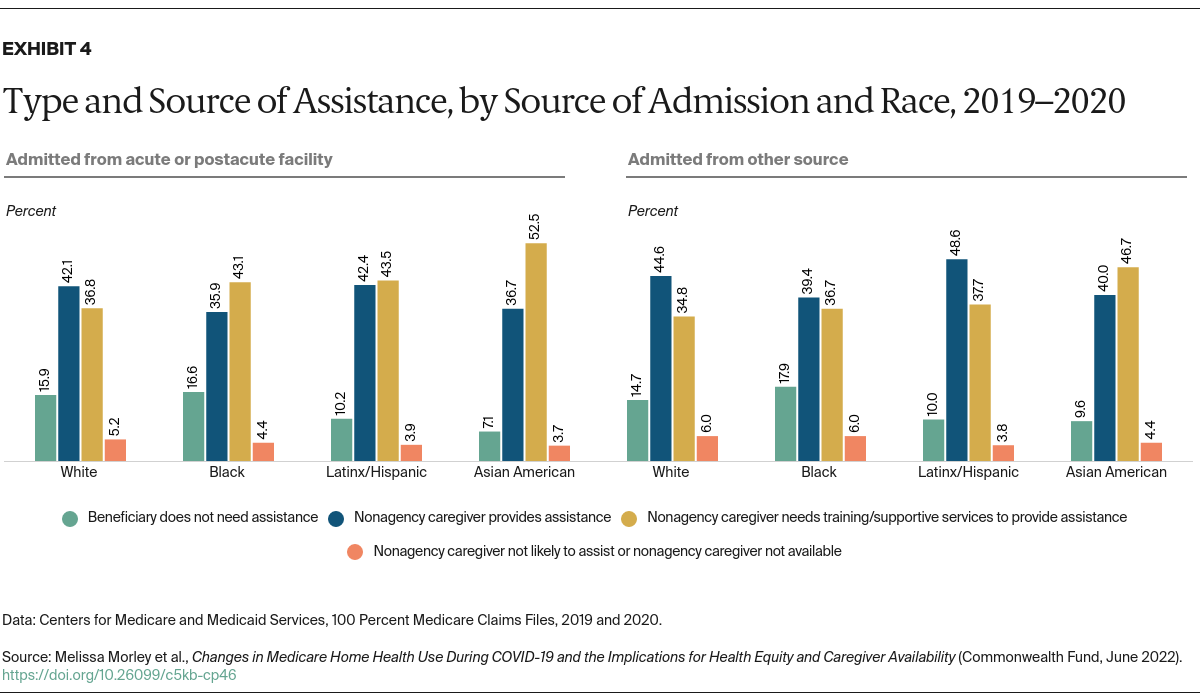
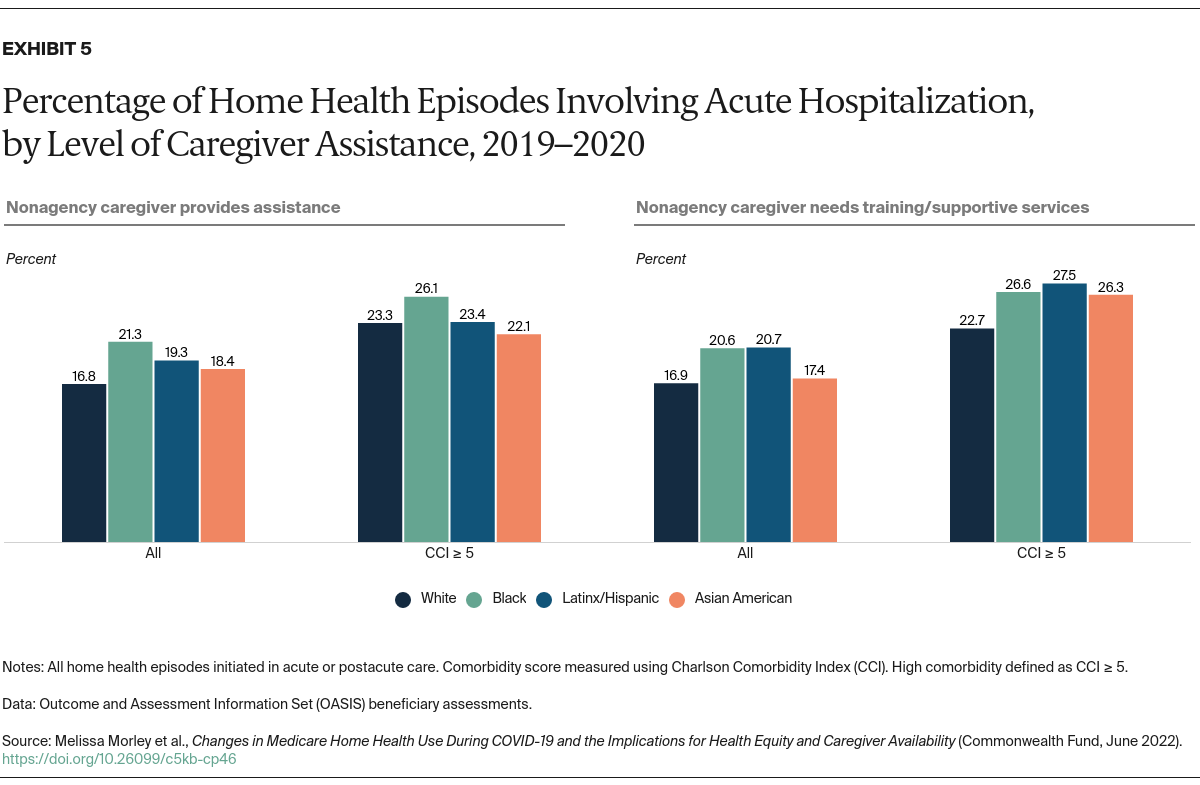
- Key Findings: Medicare beneficiaries using home health decreased by 6 percent in 2020 compared to 2019. Home health visits decreased by nearly 14 percent while patient acuity increased. Beneficiaries of color were less likely to have caregiver assistance, and a higher proportion of caregivers available to beneficiaries of color needed additional training to adequately provide assistance. Among the highest-acuity Latinx/Hispanic and Asian American beneficiaries, hospitalizations were higher when their caregivers needed training.
- Conclusion: As policymakers consider changes to the Medicare home health system, they should take into account the observed racial disparities in access to and quality of caregiver assistance, as well as the increase in patient acuity when home health visits declined.
Introduction
Home health care plays a critical role providing nursing and therapy services to patients recovering from acute hospitalizations and to frail, community-dwelling, homebound patients referred to home care by physicians. From 2002 to 2019, the number of Medicare beneficiaries using home health increased by more than 30 percent. In 2019, more than 8 percent of Medicare beneficiaries used home health care.1
The use of home health services following a hospitalization may depend on diagnoses, comorbidities, geography, and provider availability, as well as the patient’s living situation and availability of caregiver assistance to ensure safe transitions of care. In addition, home health care use may also vary by race and socioeconomic status. Recent studies have identified a lower likelihood of discharge to home health care among Latinx/Hispanic and Asian American patients relative to white patients, and higher odds of discharge to home health care among those living in socioeconomically disadvantaged and rural areas.2
Given shifting home health care patient volumes and an increasing preference for home-based care, it is important to understand the changing characteristics of the Medicare home health care patient population. In this issue brief, we discuss changes in home health users’ characteristics between 2019 and 2020, including differences in race, gender, and overall health status. We also detail shifts in service use during 2020 that may reflect both the COVID-19 pandemic and change in the home health payment system. Finally, we examine caregiver availability to learn how needs may vary by home health users’ race, health status, and outcomes.
Key Findings
Home Health Use of Medicare Beneficiaries During the Pandemic
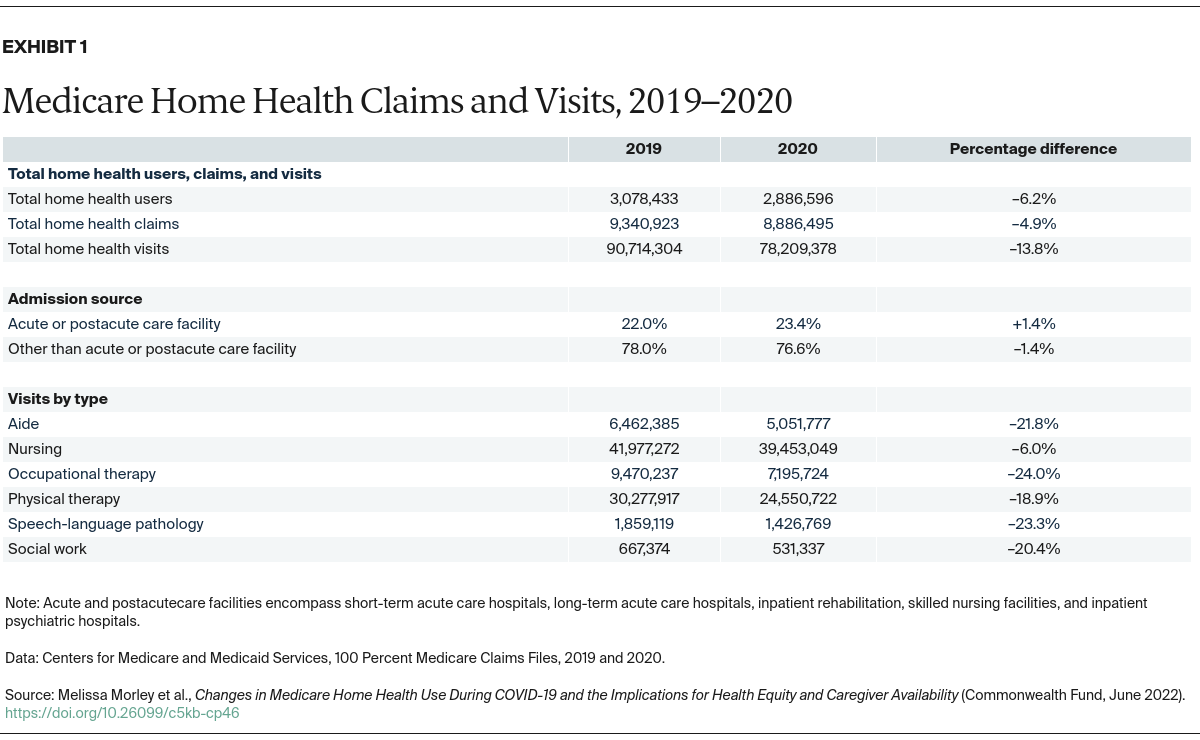
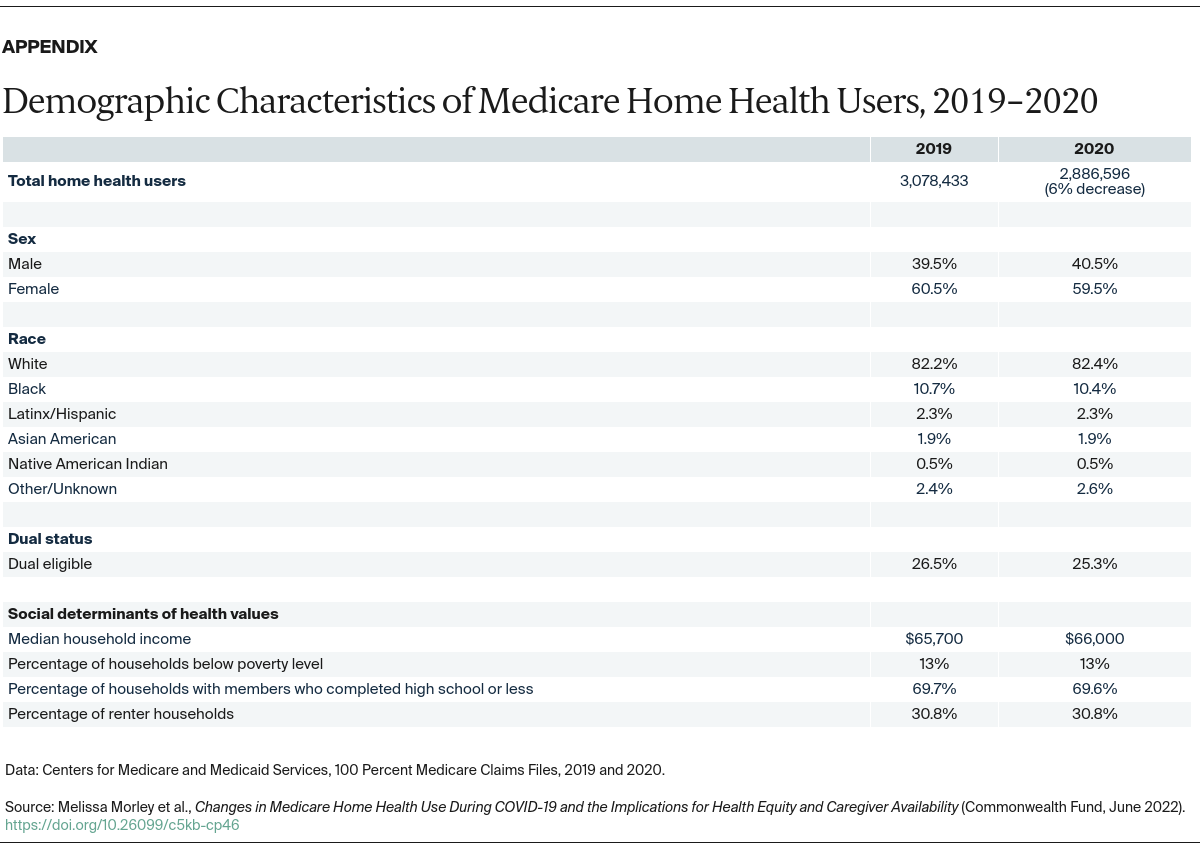
Consistent with overall trends in health care utilization during the COVID-19 pandemic, the number of Medicare beneficiaries using home health care decreased by 6 percent in 2020 compared to 2019. However, the gender and racial composition of home health users remained similar across both years (see the Appendix). Income-related characteristics of Medicare home health users also remained relatively consistent in 2020 (for example, percentage of households below poverty level).
The proportion of Medicare home health beneficiaries identified as dually eligible for Medicare and Medicaid benefits decreased slightly (0.8%) in 2020. Though a relatively small change, this finding indicates a shift in home health use among this subpopulation during the pandemic.
Types of services used. While demographics for Medicare beneficiaries using home health were quite similar in 2019 and 2020, the kinds of services received shifted notably.