Abstract
Issue: Medicare policy changes made in response to the COVID-19 pandemic may have important implications for the accessibility, quality, and affordability of mental health and substance use disorder care. Evidence is needed to inform decisions on sustaining these policies for the long term.
Goals: To characterize evidence and expert consensus on how sustaining pandemic-related Medicare policy changes might influence care and costs for beneficiaries with mental illnesses or substance use disorders.
Methods: We conducted an evidence review and a modified Delphi expert consensus process to examine experts’ opinions on whether to sustain COVID-response Medicare policies relevant to mental health or substance use disorders.
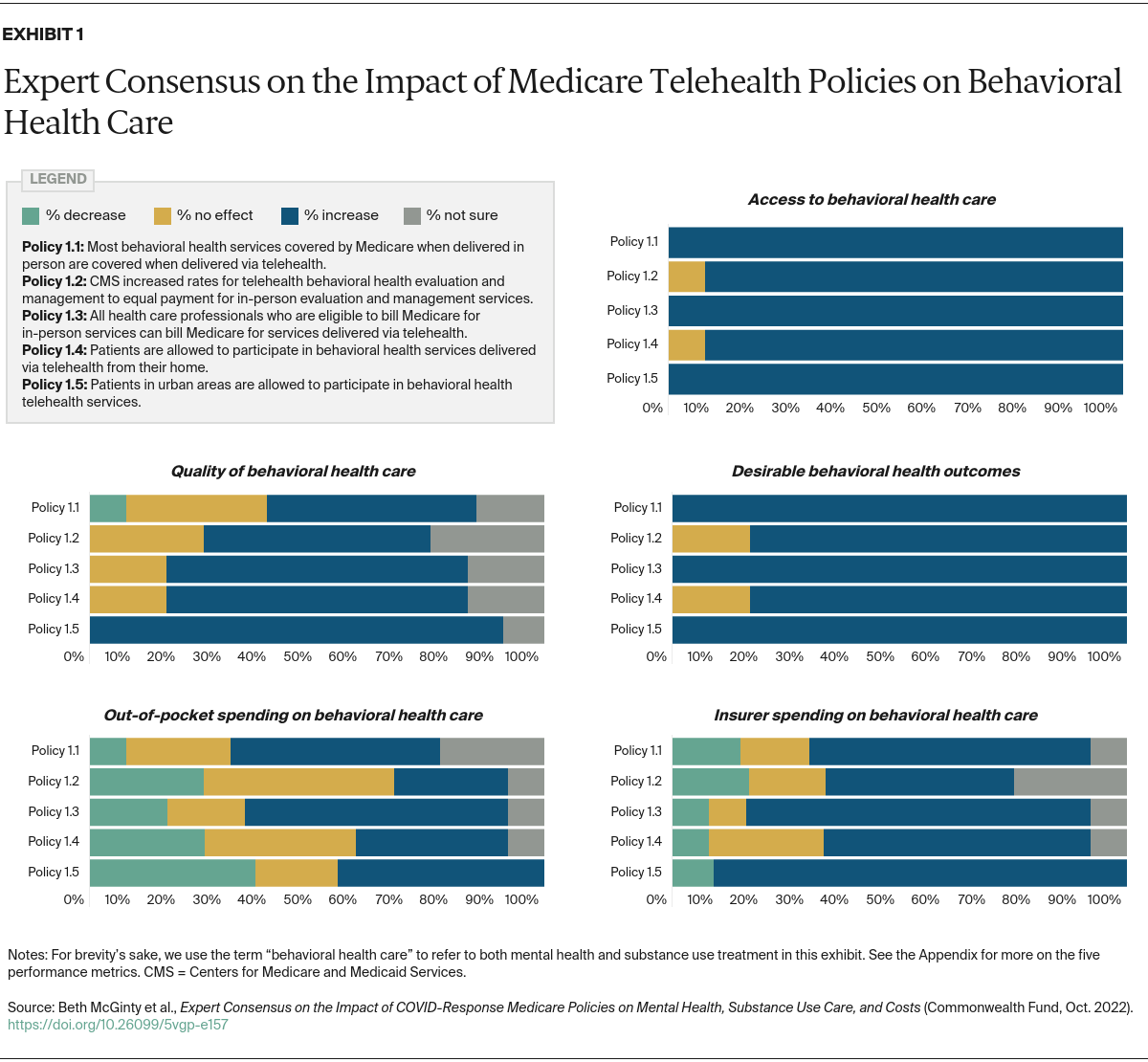
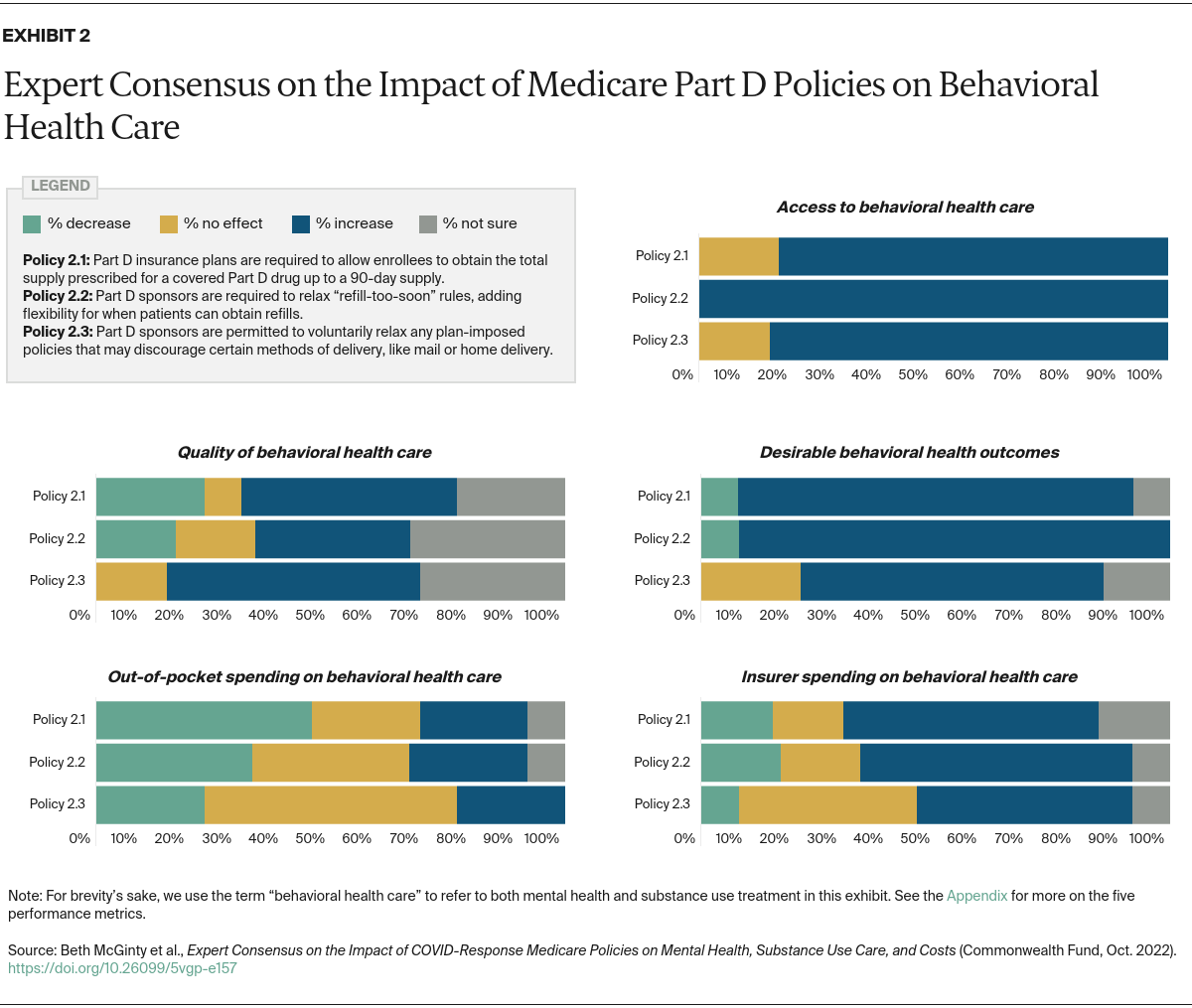
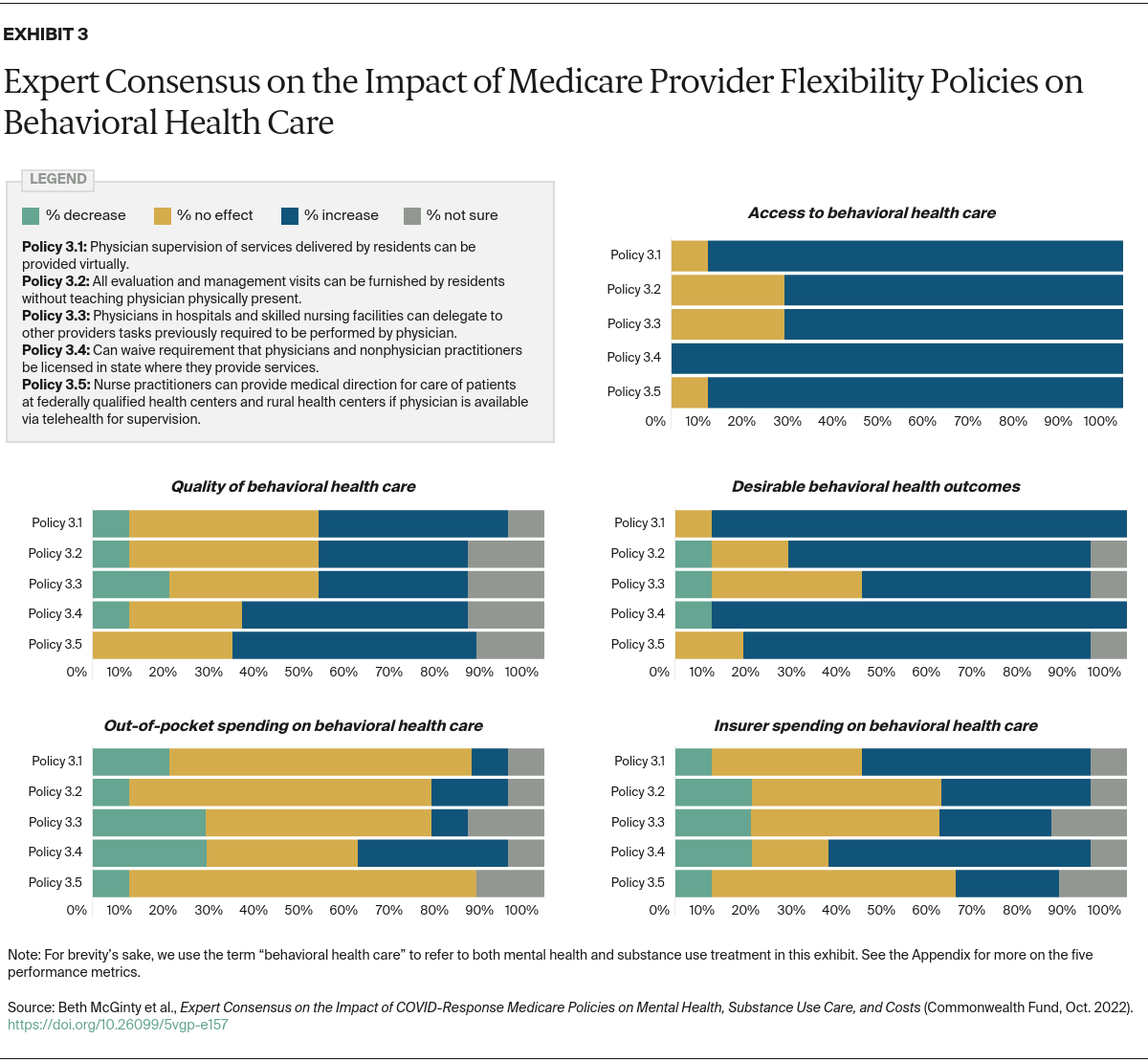
Key Findings and Conclusions: A policy waiving discharge planning requirements is likely harmful to care quality. However, policies expanding telehealth coverage, relaxing Part D restrictions, and increasing staffing flexibility likely increase Medicare beneficiaries’ access to mental health and substance use disorder care. Sustaining these three policies could improve beneficiaries’ access to mental health and substance use disorder care. Additional research is needed to understand how to best leverage these policies to achieve high-value care.
Introduction
Gaps in Medicare mental health and substance use coverage make high-quality mental health and substance use disorder care inaccessible and/or unaffordable for many beneficiaries.1 Multiple Medicare policy changes made in response to the COVID-19 pandemic — for example telehealth coverage expansions and relaxation of staffing requirements — have potentially important implications for the accessibility, quality, and affordability of mental health and substance use disorder care.2 While these policy changes were designed as short-term pandemic responses, there is ongoing dialogue regarding whether, and in what form, these COVID-related policy changes should be made permanent.
Many pandemic-driven policies are tied to the COVID-19 public health emergency issued by the U.S. Department of Health and Human Services. Some policy changes made in response to the COVID-19 public health emergency could, if sustained long term, benefit Medicare beneficiaries with mental illnesses or substance use disorders. However, other policies could have detrimental effects or unintended adverse consequences. To learn more, we reviewed evidence and sought experts’ opinions on 36 COVID-response policies that apply directly or indirectly to beneficiaries with mental health and substance use disorders (Appendix).