Medicare’s home health benefit is crucial to the welfare of beneficiaries, but its application in providing personal care leaves much room for improvement in terms of service availability and equity.
Drawing on insights from Medicaid programs’ experiences in providing personal care services, we found that: 1) a systematic approach to the referral and provision of personal care services is necessary to support equitable access; 2) separating the assessment and care plan development from the service provider helps to eliminate conflict in payment incentives; and 3) a fairly compensated direct-care workforce is required. While Medicaid programs help to fill gaps in Medicare’s coverage, restrictive and varying eligibility requirements limit its role.
Introduction
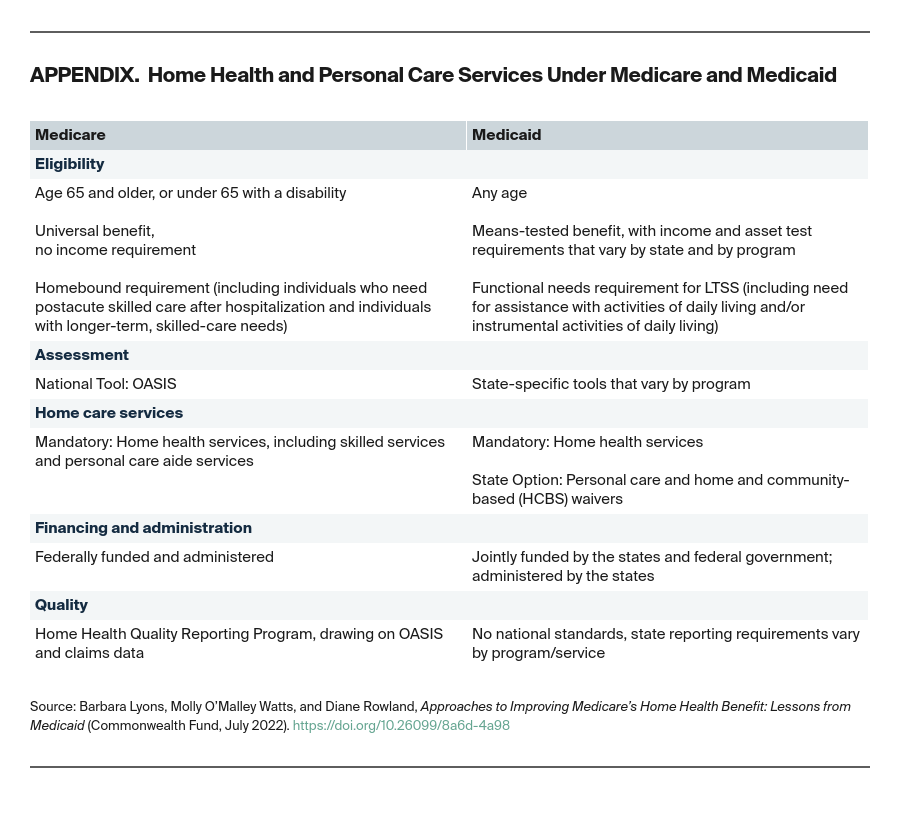
The Medicare home health benefit is designed to enable beneficiaries to receive care in their homes after hospitalizations or other acute events or for ongoing needs. It covers skilled services such as nursing and physical therapy, as well as home health aide services, including help with personal care activities like bathing, dressing, grooming, feeding, and getting around.
In practice, however, the home health benefit is falling short of its potential. Many beneficiaries are not aware of the benefit at all, many providers do not order these services for their patients, and home health agencies often do not provide the full range of services. Medicare home health visits have declined steeply over the past 20 years, and payment incentives affect who is served and how (Exhibit 1). Moreover, racial and ethnic disparities in access to these services have been documented for patients with postacute needs. When Medicare does not cover home health services, the burden of finding and paying for them is borne by individuals and their family members — often to the detriment of their health and finances.