International Approaches to Harm Reduction
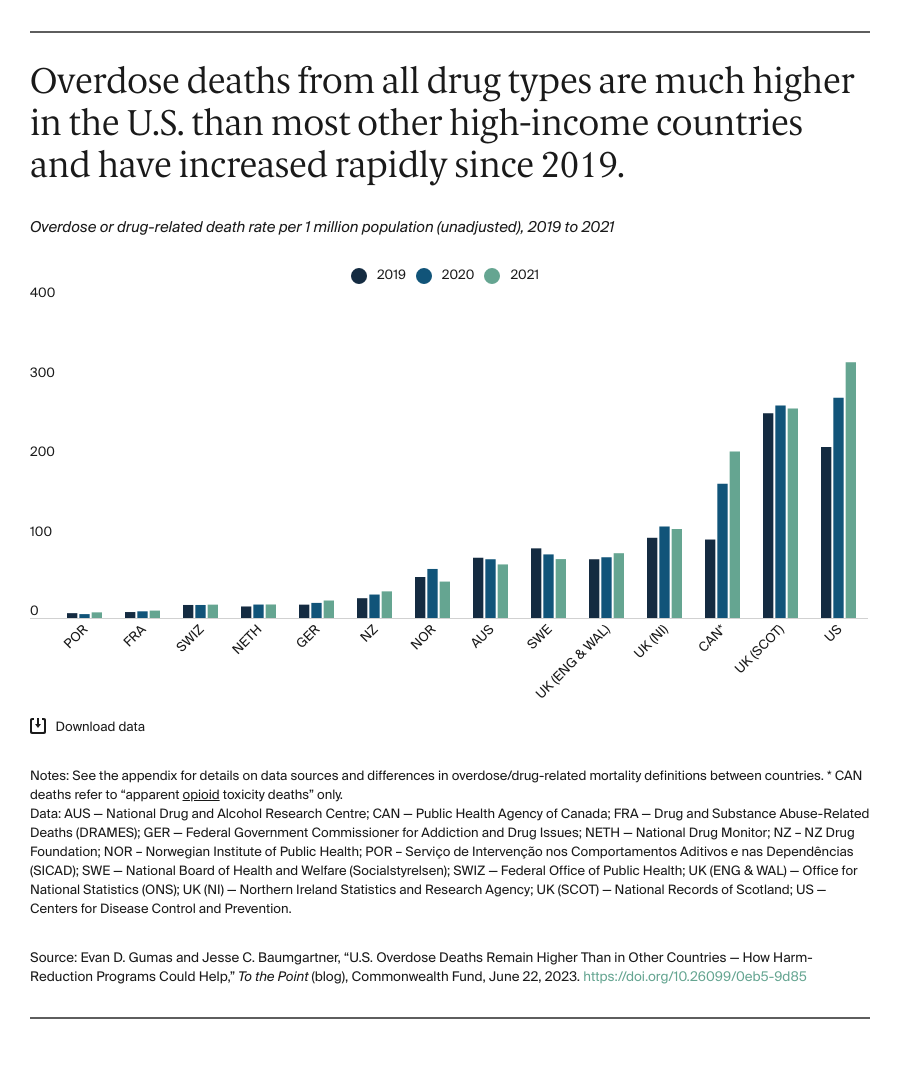
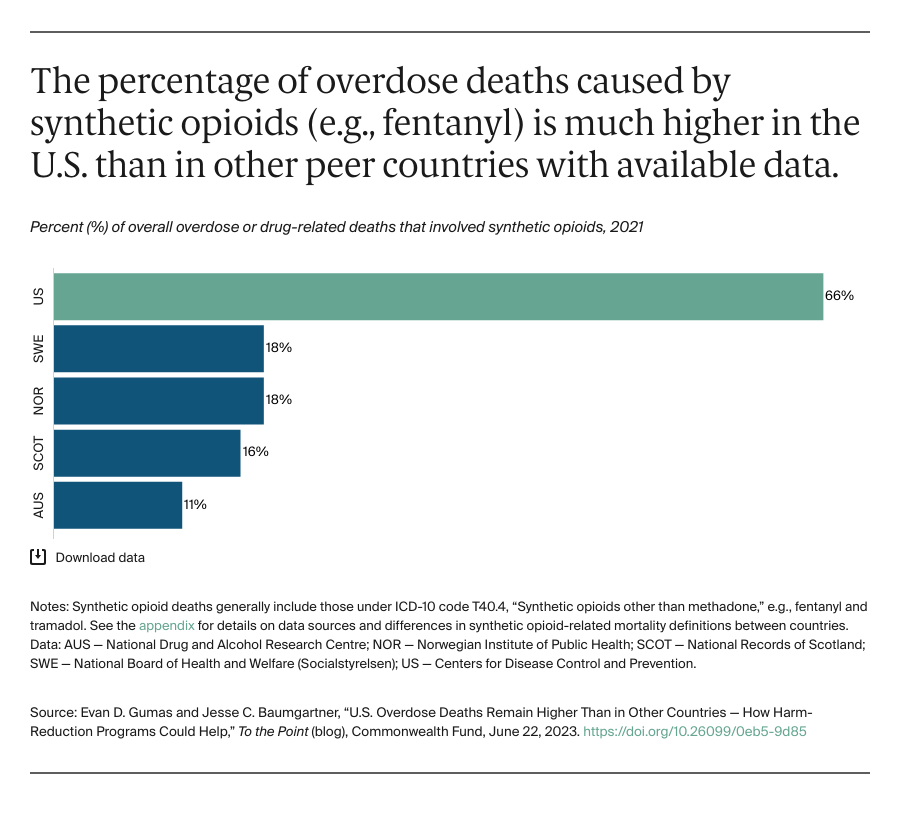
Our previous international analysis showed that access to effective addiction treatment medication is much lower in the U.S. than in other countries. In addition to access to treatment, we need harm-reduction strategies that keep people safe when they use drugs, especially given the increasingly potent drug supply. Our review of the international literature and data suggests that we can learn from other countries that report lower drug overdose mortality and make more deliberate efforts to reduce the harms of drug use and save lives.
Naloxone Access
The overdose reversal drug naloxone is critical for reducing deaths from synthetic opioids. A 2022 study showed that to counter the risk of opioid overdose almost every U.S. state would have to increase naloxone distribution, particularly through community-based organizations. Access to naloxone has improved somewhat with the recent approval of the first over-the-counter naloxone nasal spray. But barriers remain, including substantial out-of-pocket costs, differing state laws, and inadequate funding for community organizations that distribute naloxone.
Other countries, including Australia, Canada, and France, have long made it easier to access naloxone. Some cities in the U.K. offer naloxone for free while the price is minimal in France. In these countries, naloxone can be distributed to drug treatment centers, harm-reduction agencies, and more innovative community actors, like librarians. Inventive access points are also appearing in the U.S., such as vending machines in West Virginia or in nightlife venues in New York City.
Syringe Programs and Safe-Use Supplies
Syringe services programs give people who use drugs access to sterile drug-injecting equipment and reduce the harms associated with infection transmission (e.g., hepatitis C or HIV). These programs also can connect people to treatment and other safe-use tools like fentanyl testing strips and naloxone. But syringe exchange and harm-reduction services can carry stigma. In the U.S., congressional restrictions do not allow the federal government to directly fund certain activities, such as purchasing needles or syringes. Six states still have no syringe exchange programs; in some places where need is high, they’ve been shuttered. In some states, even fentanyl testing strips are criminalized.
In the Netherlands, syringe services are publicly funded and available in some pharmacies. In Portugal, the government funds and distributes comprehensive safe-use supply kits.
Diamorphine Assisted Treatment and Safer Supply
Several high-income countries, including Germany, the Netherlands, Norway, and Switzerland, have authorized providers to prescribe pharmaceutical-grade diamorphine (i.e., heroin) to people with opioid use disorder who have not responded to standard opioid addiction treatments. This additional option can offer benefits for some patients. Canada is piloting different “safer supply” programs that provide people with prescribed pharmaceutical-grade medications including opioids as an alternative to illicitly manufactured and potentially toxic drugs.
Safe Consumption Sites
Safe consumption rooms allow people to use drugs safely with supervision and connect them to treatment services. They may be used in conjunction with other tools, such as drug-checking services. There are roughly 200 safe consumption sites in 14 countries, including more than 20 in Germany. In late 2021, New York City became the first city in the U.S. to open one, with more than 700 overdose interventions through the first year. Rhode Island plans to open a center by early 2024. Recent efforts to open safe consumption sites in Pennsylvania and California have faced challenges.
Looking Forward
There has been a much higher death toll from drug overdoses in the United States than in most other countries. And yet, compared to peer nations, U.S. policymakers have placed more stringent restrictions on evidence-based models that have been shown to reduce the harms of drug use.
This may be starting to change. The Biden administration recently invested nearly $2 billion to combat the opioid crisis — including harm-reduction strategies like expanding access to naloxone and supporting syringe service programs. But these efforts fall well short of peer nations.
Moving forward, federal and state governments will need to think bigger and bolder to meet the urgency of the moment and save lives.