Introduction
In June, 67-year-old Felimon Bailon showed up in an emergency department at Presbyterian Healthcare Services in Albuquerque, New Mexico, with a large and painful abscess on his leg. The infection had been under way for nearly two weeks, turning his leg a deep purple. Doctors feared that Bailon, who is diabetic and receives oxygen therapy, might develop sepsis. They recommended admitting him to the hospital so he could receive antibiotics intravenously but he refused, insisting the infection would go away on its own if he simply took medication.
Bailon’s reaction was not unusual. For many frail, elderly patients, the prospect of being admitted to a hospital can be upsetting. It means separating from the people, pets, and familiar surroundings that create a feeling of safety. It also means disrupting the routines—a favorite meal or weekly card game—that provide joy. And, as many are probably aware, hospitalization means being at higher risk for infections, falls, delirium, functional decline, and even death.
Presbyterian, a large integrated delivery system with eight hospitals and 30 clinics, offers adult patients like Bailon who are sick enough to be hospitalized but stable enough to be treated at home that option—and more than 92 percent take it. “Hands down, it’s people’s preference,” says Karrie Decker, administrator of home and transition services at Presbyterian. To the relief of doctors, Bailon overcame his reluctance to have visitors to his home. After several daily visits and I.V. antibiotics, he fully recovered.
Presbyterian’s Hospital at Home program, launched in 2008, is based on a model developed in the mid-1990s by Bruce Leff, M.D., a geriatrician and health services researcher at Johns Hopkins University, who noticed that many of his patients suffered poor outcomes after hospital stays.1 At Johns Hopkins, teams of physicians, nurses, and other clinical staff make house calls to treat elderly patients, many of whom either refuse to go to the hospital or are at such high risk for adverse events that physicians prefer not to admit them. For select patients, this approach produces superior outcomes at a lower cost than hospital care (see Results).
The Hospital at Home model has struggled to gain traction elsewhere in the United States, however, in part because Medicare’s fee-for-service program will not pay for its services. Presbyterian is able to secure reimbursement from its health plan, which covers 470,000 Medicare Advantage, Medicaid, and commercially insured members throughout the state and has incentives to reduce costs and improve care.
Presbyterian’s program fits within a suite of services designed to deliver care in the home. These include home-based primary care, home health, hospice, and Complete Care, a care management program designed to improve coordination of services for patients with advanced illness and, when desired, avoid unwanted aggressive care at the end of life.

Hospital at Home's Target Population
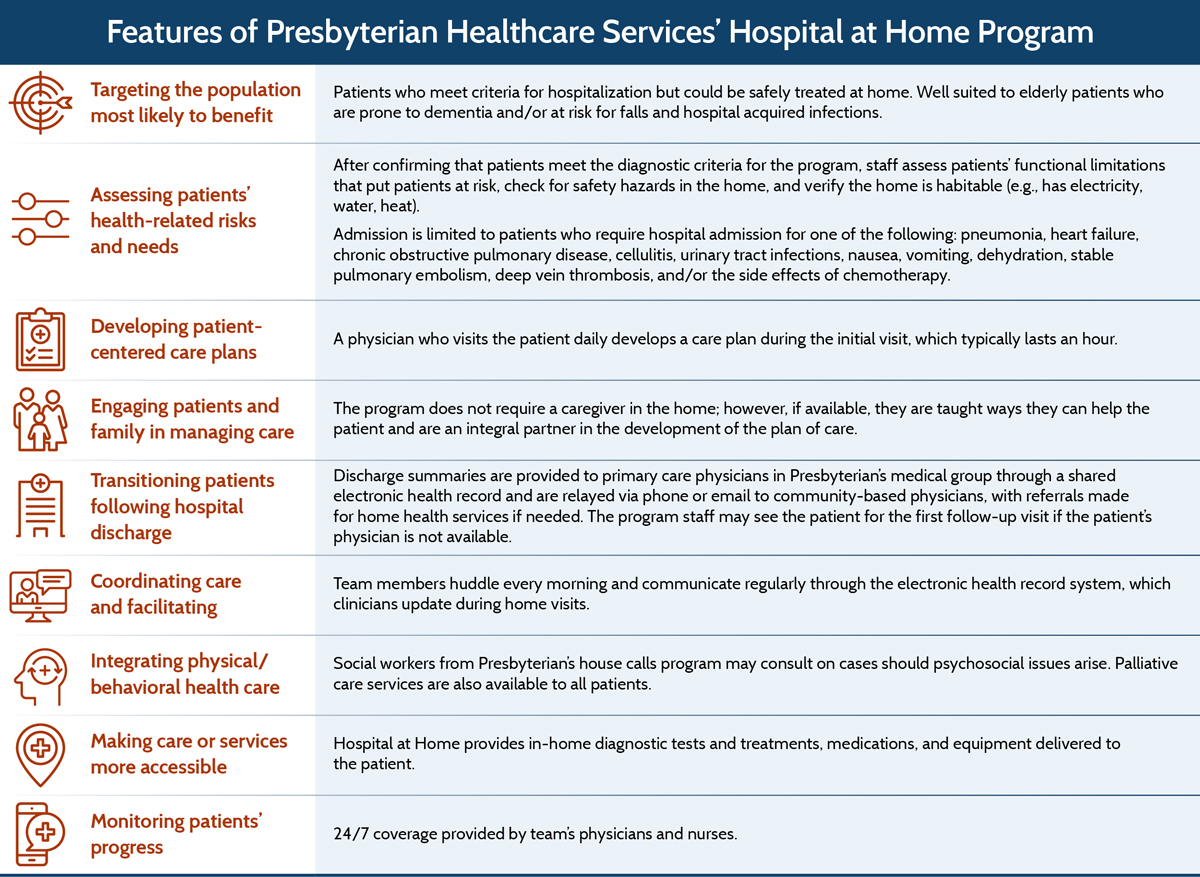
Like the Johns Hopkins model on which it is based, Presbyterian’s Hospital at Home program admits patients who have one or more specified conditions that can be safely treated in a home environment. To participate, patients must live in metropolitan Albuquerque (within 25 miles of a Presbyterian-designated emergency department) and be covered by the system’s health plan. They also must meet criteria for hospitalization established by Interqual, a proprietary tool for determining whether services are medically necessary.
Since 2008, the program has treated more than 1,200 patients with a range of clinical characteristics and an average age of 77. The program treats about two patients a day.
Key Program Features
Identifying Appropriate Patients
Patients enter the program in a variety of ways: as transfers from Presbyterian’s emergency departments (EDs) and hospitals; through referrals from primary care doctors, specialists, and urgent care facilities; and via referrals from Presbyterian’s home health agency and its house calls and Complete Care programs. Ideally, patients receive referrals for at-home hospital services before they have reached the ED. By that point, patients and families are often exhausted, making a transfer back home less appealing.
Before admitting a patient to the program, staff verify that the patient’s home environment will support treatment—for example, it has basic utilities. “Safety is really important,” says Melanie Van Amsterdam, M.D., one of two physicians making home visits. They also assess the patients’ functioning, making sure they can walk and get to the bathroom. The program does not require that a caregiver be present in the home.
In all cases, Presbyterian’s goal is to distinguish patients who truly need hospital-level care at home from those who could benefit from less-intensive oversight through its home health, hospice, and palliative service programs.
Extended Home Visits

While the average length of stay for Presbyterian patients who receive Hospital at Home care is shorter than that for hospitalized patients (3.2 vs. 4.11 days), such patients typically have more face-to-face time with clinicians. Physicians, who visit once daily, may spend up to an hour with patients on assessment, diagnosis, treatment, and care planning. Nurses may spend up to two hours with patients once or twice a day to administer infusions and medications, conduct lab tests, and provide education to patients and their families. Home health aides also may spend up to an hour a day in the home helping to bathe patients, and prepare light meals if needed. When needed, Presbyterian also sends social workers and rehabilitation specialists (including occupational therapists, physical therapists, and speech therapists).
Spending more one-on-one time with patients allows clinicians to get to know them better and have in-depth conversations, says Van Amsterdam. “We’re on their territory and patients are much more vocal about what they want and what they will and will not do,” she says. In contrast, “in the five or 10 minutes a hospitalist spends with them in the hospital, they may say, ‘Yes, doctor.’ But when they are at home they will say, ‘I have no idea what you just said.’”
Being in the home also allows providers to see the problems patients face coping with their disease, including managing their medications and maintaining a healthy diet. “[We’ll find] bags of medications and supplements that are outdated—they may be someone else’s from five years ago,” she says. In one case, a caregiver discovered a patient was taking his son-in-law’s medication instead of his own—a 600-milligram dose instead of the 100 milligrams he was prescribed. As a result, he was sleepy, dizzy, and occasionally falling. A home visit also gives providers time to review what patients are eating and negotiate manageable changes in diet. For a patient with congestive heart failure, this can mean eating a smaller portion of lox at breakfast to reduce salt intake.
Providers discharge patients from the program using the same criteria that hospitals use. Discharge summaries are sent to primary care physicians in Presbyterian’s medical group through the shared electronic medical record system, or relayed by phone or email if a patient has a non-Presbyterian primary care physician. To promote continuity of care, Hospital at Home staff may provide the first follow-up visit after discharge, and program nurses may continue to see patients who receive home health services.
Rapid Response
I think people have more dignity [when they receive care at home]. They have control over their medication. They don’t have people coming in and out to take their blood pressure, and they’re not in hospital gowns. They’re in their own clothes and have privacy.
The program’s narrow geographic radius helps to ensure physicians and nurses can get to a patient’s home within a half-hour should a patient’s symptoms worsen. A response time of two hours or less is required from vendors who deliver durable medical equipment, intravenous medication, oxygen, ultrasound, mobile X-ray technology, and electrocardiogram equipment.
Because the daily census fluctuates and patient needs vary, ensuring adequate staff can be tricky. “If you have five patients, and three of them have twice-daily IV infusions and they live in three different counties, then you’re going to have to be very creative” in planning and prioritizing visits, Van Amsterdam says.
A Continuum of Care
While Presbyterian’s home health, hospice, primary care house call, and Complete Care programs operate largely independently—rarely sharing staff—they frequently make referrals to one another. This enables providers to respond quickly when a patient shows signs of deterioration.
Having complementary business lines also made the process of developing them easier. “It’s not an easy build,” Leff says of Hospital at Home programs generally. “The implementation is always dependent on highly local factors. For instance, you have to be able to get IV meds to the home, and every place you implement Hospital at Home there’s going to be a slightly different way of doing that.” Presbyterian convened 12 interdisciplinary teams to create the processes needed to roll out the service lines, build physician support, and find ways to increase patient awareness of Hospital at Home.
a Personal communication with Presbyterian Healthcare Services, May 27, 2016.
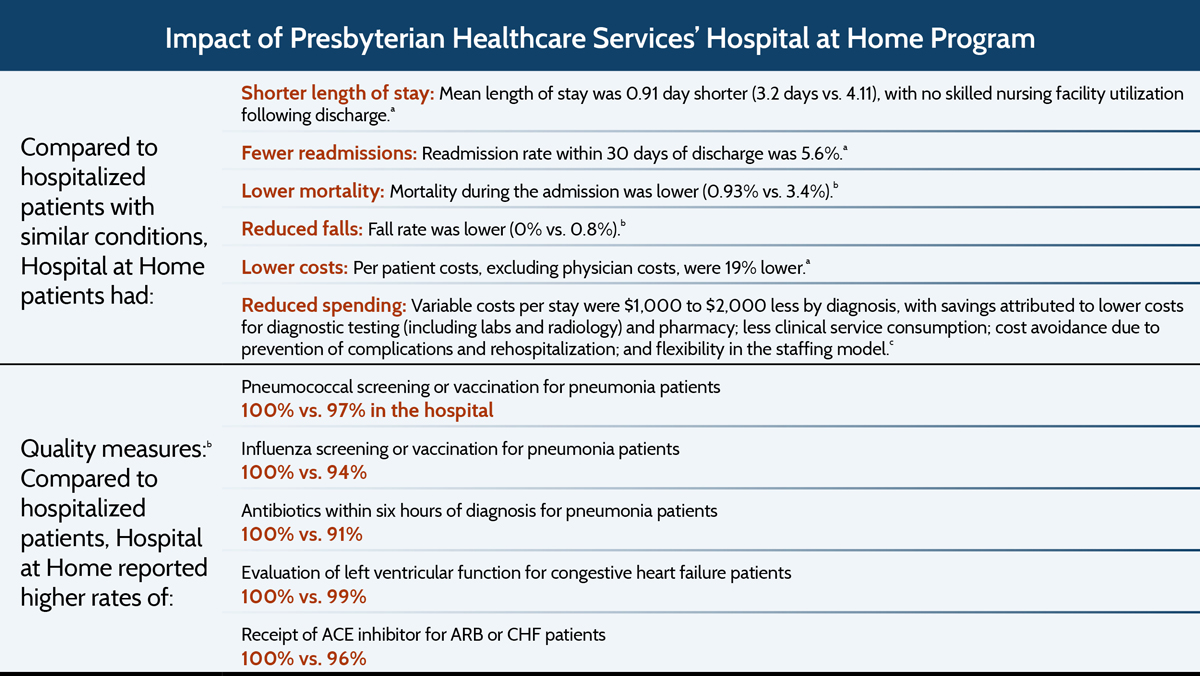
b Presbyterian Healthcare Services and L. Cryer, S. B. Shannon, M. Van Amsterdam et al., “Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients,” Health Affairs, June 2012 31(6):1237–43.
c V. Foubister, “Hospital at Home Program in New Mexico Improves Care Quality and Patient Satisfaction While Reducing Costs,” Quality Matters, Aug./Sept. 2011.
Financing
Presbyterian’s health plan pays the Hospital at Home program a bundled rate for each admission, based on diagnosis codes (calculated as a discount of Medicare’s Prospective Payment System rates). The payment covers fees for provider visits, nursing visits, home health aide visits, ancillary services such as durable medical equipment, and diagnostic tests. The vast majority of patients (90%) are covered by Presbyterian’s Medicare Advantage plan; the rest are covered by its commercial health plan. It cannot bill for its service under traditional fee-for-service Medicare or Medicaid, a factor that limits the size of the program.
Results
A national demonstration of Johns Hopkins’ Hospital at Home model conducted in 2001 and 2002 in Medicare managed care plans and the Veterans Administration found that providing acute-level care at home for a discrete set of conditions was not only significantly cheaper—by 32 percent—but safer as well, owing to a dramatically lower incidence of delirium, among other complications.2 Two meta-analyses of randomized controlled trials of Hospital at Home programs came to similar conclusions: they found that patients treated at home instead of the hospital had lower mortality rates and lower costs. Patient satisfaction was higher as well, as patients remained close to their support networks and had less disruption to their lives.3

Insights and Lessons Learned
Finding the right staff can be challenging. At Presbyterian, finding physicians who are the right fit for the program proved harder than expected. They need to be comfortable with the independence, the time on the road, and the unpredictable tempo of the job. Hospitalists—who are accustomed to managing hospitalizations from start to finish—seemed like a logical choice. But Karen Thompson, who directs both the Hospital at Home program and Presbyterian’s hospice program, says that while they loved the concept of the program, many felt they would be uncomfortable treating patients without immediate access to the resources of the hospital—including CT scanners, immediate lab results, and other staff. The program has had more success recruiting primary care physicians like Van Amsterdam, who sought out the job because she wanted to spend more time with patients than the 20 minutes scheduled in primary care practices.
Presbyterian administrators also have found that nurses who’ve worked in EDs or critical care units—accustomed to making decisions based on quickly changing circumstances—are a better fit for Hospital at Home than are home health nurses. The nurses they ultimately hired “are all very skilled at clinical assessment,” says Darren Maestas, R.N., patient care manager, who had previously worked for a regional hospital as director of medical, surgical, and intensive care services and has several years of experience in home health.
To support the required staffing and infrastructure, Hospital at Home programs need to draw on a critical mass of patients. Because only a fraction of patients needing acute care qualify for Hospital at Home as currently designed, such programs may be more viable in larger urban areas where a sufficient and predictable number of patients can be enrolled. Decker estimates that metropolitan areas of 5 million or more people might provide enough economy of scale to support a full-time team treating at least five or six patients a day.
Presbyterian sometimes falls short of this number in its smaller metropolitan market, making it important to embed the program in a larger suite of continuing care services. Using Hospital at Home programs as alternatives to observation stays, subacute care, or postsurgical care may be another way to increase the patient census. “We do sometimes branch out,” Van Amsterdam says. “There have been occasions when the health plan has come to us and said, ‘Could you just take these influenza patients? Because they don’t need to be in the hospital but do need to be monitored, and they need support in the home.’”
Payment and medical culture may be barriers to spread of this model. Payment is likely to remain a barrier to the spread of hospital care delivered at home unless and until this service become reimbursable under fee-for-service Medicare and Medicaid. Paying through Medicare Advantage or accountable care contracts is an option, but this would require a high degree of market penetration to yield the volume of patients needed in any given region.
Variations of Hospital at Home programs have been more successful in countries where government controls both the funding and delivery systems, such as Australia and England, and in facilities run by the U.S. Veterans Health Administration, which has been able to successfully implement programs at 11 sites.4,5 Even when payment and delivery system incentives are aligned, however, many programs here and overseas continue to encounter some resistance from referring physicians who are concerned about safety and liability risks. With experience, they usually become more comfortable with the idea, but it takes time.




