Introduction
Sylvia Trujillo was so desperate to have her 68-year-old mother Carolyn enrolled in MedStar Washington Hospital Center’s Medical House Call Program that she moved from one part of the District of Columbia to another—just to be in the program’s catchment area. In the years leading up to the move, her mother was in and out of the hospital every month or so as Trujillo struggled to find a physician who could manage her multiple chronic conditions. These included diabetes, depression, and early dementia, as well as a rare genetic disorder that led to a host of health problems, including multiple falls. “She easily saw 20 to 30 different physicians, because no one could figure out what was going on,” Trujillo says.
Patients like Trujillo’s mother were the inspiration for MedStar’s Medical House Call program, launched in 1999 by two geriatricians troubled by the quality of care received by patients who were too sick, frail, or disabled to visit doctors’ offices. Too often, the burden of caring for such patients fell on overwhelmed family members or friends struggling to keep up with their needs. Even worse off were patients with no family nearby. “No one knew they were getting sick, and no one was there to prevent the cascade of crises that land patients in the emergency department or hospital,” says George Taler, M.D., MedStar’s director of long-term care and one of the program’s founders.
MedStar’s program offers round-the-clock access to a care team comprising a geriatrician, nurse practitioner, and social worker. The house calls reveal and address problems that are missed when care is poorly coordinated, enabling team members to identify social supports for patients that can improve quality of life, reduce the burden on caregivers, and head off problems that can lead to high-cost institutional care.
Based on the cost savings it achieved, the program became one of the models for the federal Center for Medicare and Medicaid Innovation’s Independence at Home Demonstration, which is testing whether providing primary care at home to frail elderly patients with multiple chronic conditions or advanced illnesses improves outcomes and lowers health care spending. MedStar participates in the demonstration as part of a consortium that includes Virginia Commonwealth University and University of Pennsylvania Health System, both of which are implementing an approach similar to MedStar’s. The consortium is one of nine participating groups to earn a share of the savings they produced for Medicare.

Medical House Call's Target Population
On a daily basis, the Medical House Call Program serves an average of 600 frail elderly patients, most of whom live within the District of Columbia. The majority rely on MedStar Washington Hospital Center for hospital care. One-third participate in the Independence at Home Demonstration. The remainder are covered by Medicare, Medicaid, and commercial insurers. The program’s eligibility criteria are designed to identify patients at the greatest risk of incurring high costs, and thus go beyond criteria used by other payers for home-based primary care.
MedStar serves a predominantly poor population. On average, patients in the program have between two and three chronic conditions. More than half (58%) suffer from Alzheimer’s or chronic mental illness. Other common conditions include severe arthritis (40%), congestive heart failure (38%), diabetes (36%), and chronic obstructive pulmonary disease (22%). Approximately 90 percent are African American, and three-quarters are women.1
Key Program Features
Team-Based Primary Care
MedStar’s team-based approach to primary care begins with an at-home assessment provided by a geriatrician. Lasting from one to two hours, the assessment is used to identify the constellation of clinical, psychological, and social problems the patient is facing, as well as medication discrepancies and safety hazards. In homes where a caregiver is present, typically half the visit is spent with the patient discussing physical symptoms such as pain or difficulty breathing. The other half is spent listening to the caregiver’s concerns, like how to safely move a patient or how to deal with a dementia patient who wanders at night.
Based on the outcomes, an interdisciplinary team that includes the geriatrician, a nurse practitioner, social worker, and a licensed practical nurse establishes and shares responsibility for implementing a plan of care. The team meets for two hours weekly to discuss patients with unstable conditions and gather input from consulting pharmacists, physical therapists, psychiatrists, and other specialists. Representatives of home health agencies are also engaged, as needed.
The staffer overseeing the most pressing care needs typically takes the lead in orchestrating the care plan—the geriatrician, if medical issues are most urgent; a nurse practitioner, if medical needs are less urgent; or a social worker, if psychological or social supports are the priority. “We don’t have care managers or case managers,” says K. Eric De Jonge, M.D., associate professor of clinical medicine, geriatrics, and long-term care at Georgetown University School of Medicine, and the program’s other cofounder. “Whichever problems are the most complex or acute, that discipline tends to be in charge.”
Team members rely on a mobile electronic health record to coordinate care. They also have access to CRISP, a regional health insurance exchange that allows them to track the 10 to 20 percent of patients who were admitted to hospitals other than Medstar Washington Hospital Center. The system also flags emergency department use.
Responsiveness to Patient Needs
Geriatricians provide 24/7 on-call coverage as well as guidance to nurse practitioners, who visit patients anywhere from several times a week to once every eight weeks. As required by the demonstration, the nurse practitioners make home visits within 48 hours of a hospital discharge and within 24 hours should a patient need urgent care (these visits often occur within two to four hours during the work week). In-home diagnostic tests and treatments, medications, and equipment are delivered to the patient.
Team members have become adept at recognizing problems that would be of concern to their colleagues, Taler, MedStar’s long-term care director, says. “The medical staff can identify social problems and the social worker can identify medical issues. That’s a core element of how we prevent crises.”
On occasion, team members make joint visits to resolve conflicts in the care plan, ethical questions, or safety concerns, including worries about elder abuse, mental capacity, or the safety of providers in the home. “We’ve had family meetings with seven disciplines in the room,” De Jonge says.
Focus on Emotional Needs of Patients and Families
Social workers are actively involved with about a third of MedStar’s cases, providing education, emotional support, and counseling to patients and their caregivers. This may include peer support and referral to resources such as adult protective services, bill-paying assistance, and legal services. Arranging for home health aides and respite care has also been essential to preventing caregiver burnout, which is one of the reasons De Jonge views social services and psychological support as equal in importance to medical management.
Providing skills-training and support to caregivers, who may panic when their family member has difficulty breathing or is in pain, also lessens reliance on hospitals and emergency departments. “The patients who have great, devoted, open, responsive caregivers are the ones who almost never show up at the hospital, because they are willing to work with us, do things at home, wait for us to arrive, and then implement the plan of care,” he says.
MedStar also created peer-support groups and a prayer line for families.
Continuity of Care
Geriatricians oversee the care of patients when they are hospitalized. This enables them to stay apprised of patients’ evolving needs and ensure that hospital staff adhere to patients’ preferences. For hospitalizations resulting from a fall and fracture, care is provided by MedStar’s OrthoGeriatrics hospital team, which includes geriatric, orthopedic, rehabilitation, and nursing care professionals. Under that service line, the house call program’s geriatricians help to manage chronic conditions so they do not worsen while other doctors are focusing on the patient’s orthopedic needs.
Emphasis on End-of-Life Care
The trusting relationships that develop between team members and patients and their families facilitate frank discussions about the care patients wish to receive at the end of life. “Every family and patient is different in terms of what their spiritual beliefs are and how much invasive care they want,” De Jonge says. “You have to get to know them and have them trust you. So [when Dr. Taler] comes in and says…‘We’re not helping your mom anymore—we’re hurting her,’ they trust him.” The conversation can then turn to maximizing the patient’s comfort and meeting her and the family’s expectations for a ‘good death.’
The long-term trust you build by visiting people at home and understanding their values and their religion and wishes allow us to advocate for them when they’ve reached the end of life. We can then pick a path with them that is consistent with those values, whether it is one last try in the ICU or whether it is just letting them stay at home.
In MedStar’s house calls program, 60 percent of patients die at home, while 25 percent die in the hospital and 15 percent in inpatient hospice programs. This is in contrast to national studies finding that about 70 percent of African Americans die in hospitals while only 6 percent die at home. “Our patients die where they want, with dignity and comfort. They also happen to not be in super-high-cost institutions,” Taler says.
Financing
The program, which was initially launched with grant funding and support from the hospital, bills Medicare and Medicaid on a per-service basis. This amounts to roughly $100 per visit. Under the Medicare demonstration, the program continues to receive fee-for-service payments but shares in any savings that result from lower utilization of health care services, provided the care meets Medicare quality standards. MedStar is now in discussions with a Medicare Advantage plan to provide at-home primary care to the plan’s highest-risk patients on a capitated (lump-sum-payment) basis, amounting to roughly $300 or $400 a month. There is also the possibility of shared savings for meeting quality benchmarks.
Results
In the first year of the Independence at Home demonstration, the consortium reduced Medicare spending by 20 percent relative to expected spending for that population ($4,060 vs. $5,076). This yielded just over $1.8 million in shared savings, to be split among the three partners.2 (Some of the savings allowed the consortium to recoup the $300,000 it had invested over two years to pay for a data analyst and hire additional staff to provide care on Saturdays.)
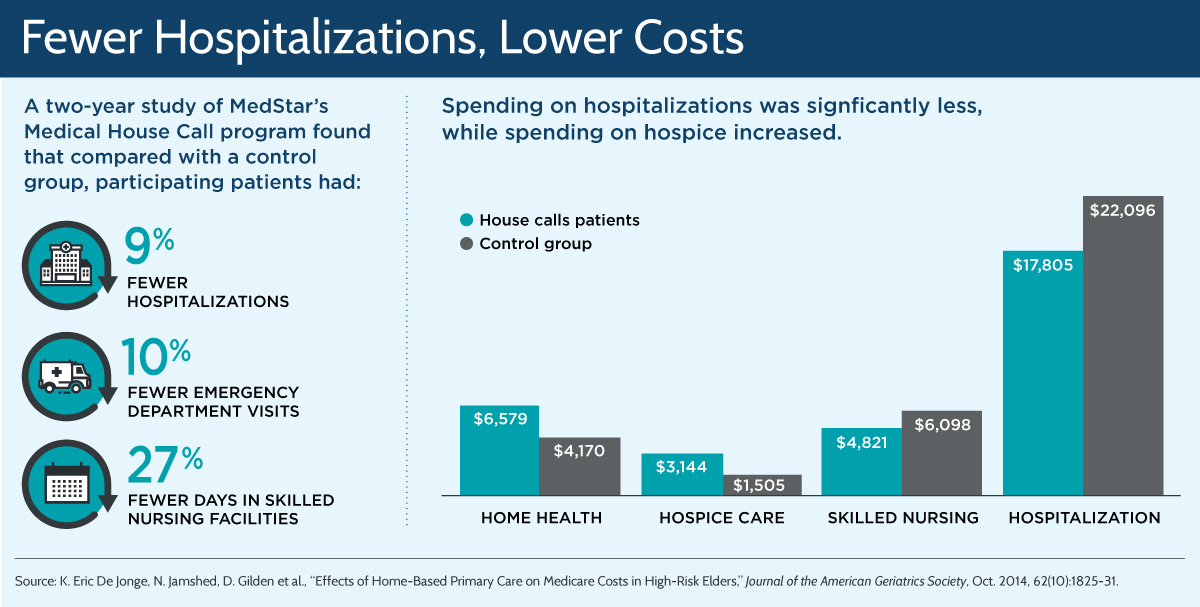
The magnitude of these savings is similar to those reported in a published study that compared Medicare patients in MedStar’s program with a case-controlled group of fee-for-service Medicare beneficiaries between 2004 and 2008.3 Costs of care and the use of hospitals, emergency departments, and skilled nursing facilities declined, while spending on hospice and home health services increased. After controlling for potentially confounding factors, total savings were 17 percent for all patients in the program, and 26 percent for those in the highest risk category based on measures of frailty, while mortality rates were similar for both groups.
Insights and Lessons Learned
Home-based primary care shows potential but is currently limited in scale. While nine of the 14 Independence at Home Demonstration participants have had success—with one achieving total savings of 32 percent in the first year—the program has been limited in its effect, because Medicare has capped participation in the program at 10,000 beneficiaries. Legislation converting the demonstration into a permanent Medicare benefit was pending in the U.S. Senate as of July 2016.4
Workforce shortages may limit the model’s spread. Finding geriatricians and other physicians accustomed to providing care at home is a limiting factor at the local level, one that is hard to overcome. The American Geriatrics Society projects that as the U.S. population ages, the country will need 30,000 geriatricians by 2030; by comparison, there were fewer than 6,800 in 2010.5 One of the reasons for the shortage is that geriatricians tend to be at the bottom of the pay scale, Taler says.
The kind of shared savings generated by the demonstration could help address this shortage—if the model were expanded nationally. MedStar is using part of its share to boost salaries by 10 to 15 percent. If others could do the same, “that could change the entire ball game,” Taler says. He notes that primary care physicians, with some additional training and on-the job experience, could help fill the gap. Anticipating this need, the Schaumburg, Ill.–based Home Centered Care Institute has developed a house calls training program for physicians.
Narrowing the program’s focus to the highest-risk patients uncovers the greatest opportunities for care improvement and cost savings. MedStar’s experience demonstrates the benefit of devoting resources to the sickest patients. “It runs counter to the common wisdom, which is that once people get too sick there’s not too much you can do to help them. What we found is just the opposite: the sicker and frailer the patient, the more you can impact their needs if you have the right system,” Taler says.
This was born out in the case of Sylvia Trujillo’s mother. Home visits from the team of providers who coordinated her care changed the lives of both mother and daughter. With the MedStar team gradually reducing her medications and addressing small problems before they became big ones, Trujillo’s mother steadily improved. In fact, in the last year, she was hospitalized only once. "One day, I'm going to add up all the money this program saved Medicare," Trujillo says.


