Background
Stress echocardiography, or annual stress cardiac imaging, is one of the most frequently ordered diagnostic tests in Ontario and across Canada. “It is a big line item on provincial health care budgets,” says Kevin Levitt, M.D., a Toronto cardiologist. The Canadian Cardiovascular Society Choosing Wisely Canada list counsels against routine stress echocardiography, which helps determine if there are arterial blockages in the heart that might affect blood flow to the heart. Asymptomatic, low-risk patients account for up to 45 percent of unnecessary screening. The recommendation asserts that the screening should only be done on patients with specific risk factors like high blood pressure or smoking, or a medical history of heart disease.
Levitt cited a number of drivers for this project. First, there was a long waitlist for patients for stress echocardiography, with patients who do not necessarily need the test making the wait longer for those who require timely testing. Second, positive results (including false positives) are usually followed up by an angiogram, a more invasive cardiac test, which can affect patient care and health care system costs.
The Innovation
Dr. Levitt launched a hospitalwide implementation effort to reduce unnecessary stress echocardiography ordered by physicians at St. Michael’s Hospital in Toronto. His goals were to shorten the waitlist for a stress echocardiography for patients who truly needed it, and help patients avoid false-positive results that are followed up by more invasive cardiac tests like cardiac catheterization or medication. The intervention included 425 patients referred for a stress echocardiography.
Population Targeted
Patients referred for stress echocardiography at St. Michael’s Hospital, a large 550-bed tertiary care hospital in Toronto; and clinicians who order this test, including family physicians, internists, surgeons, cardiologists, and anaesthesiologists.
Key Features of the Innovation
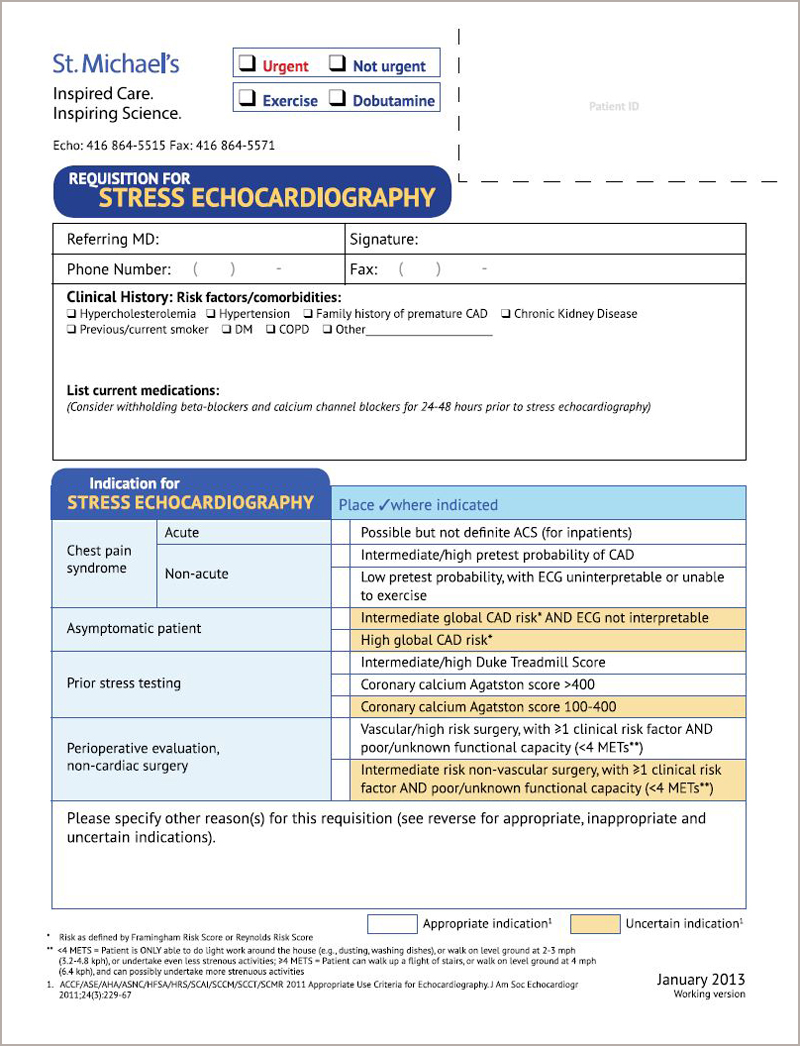
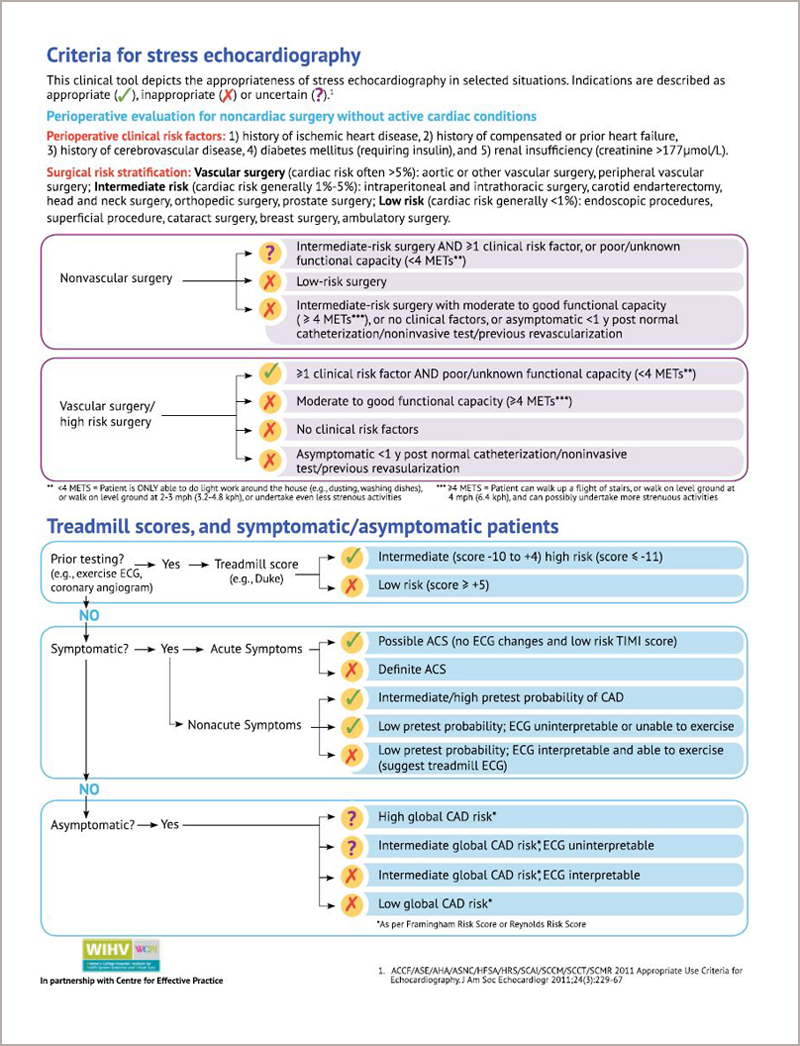
The intervention centered on the development of a decision-support tool, or form, that clinicians were required to complete to order a stress echocardiography at St. Michael’s. Steps in launching the tool included:
- Convening a focus group of physicians who most commonly order stress echocardiography studies to discuss the nuances and reasons for inappropriate ordering. This focus group served two purposes: educating clinicians about the harms to patients of unnecessary stress echocardiography tests, and gathering input for the decision-support tool.
- Facilitating a review of the tool by clinicians and a graphic designer to ensure ease of use and ability to integrate into the workflow of busy clinicians.
- Integrating the tool into practice and requiring any physician who wished to order a stress echocardiography test to complete it.
A study of the intervention found a reduction in “rarely appropriate” stress echocardiography from 31% to 19%.
Evidence of Impact
A study of the intervention, published in 2014 in the Journal of the American Society of Echocardiography, found a reduction in “rarely appropriate” stress echocardiography from 31 percent to 19 percent. Levitt notes that a challenge to sustaining this intervention today is that it was introduced in a paper-based system. He suggests that the form now be integrated into hospitals’ electronic medical record systems.
Sharing and Spreading the Innovation
Since this study was published, researchers collaborating with Choosing Wisely Canada have conducted additional studies on interventions to reduce unnecessary cardiac testing in Ontario. For example, the Echo WISELY trial was published in the Journal of the American College of Cardiology in 2017. This clinical trial tested an educational intervention directly delivered to physicians to supplement decision-support tools and forms to reduce unnecessary cardiac testing.
Contact for Further Information
Dr. Kevin Levitt, Cardiologist, Michael Garron Hospital, Toronto, [email protected]


