Introduction
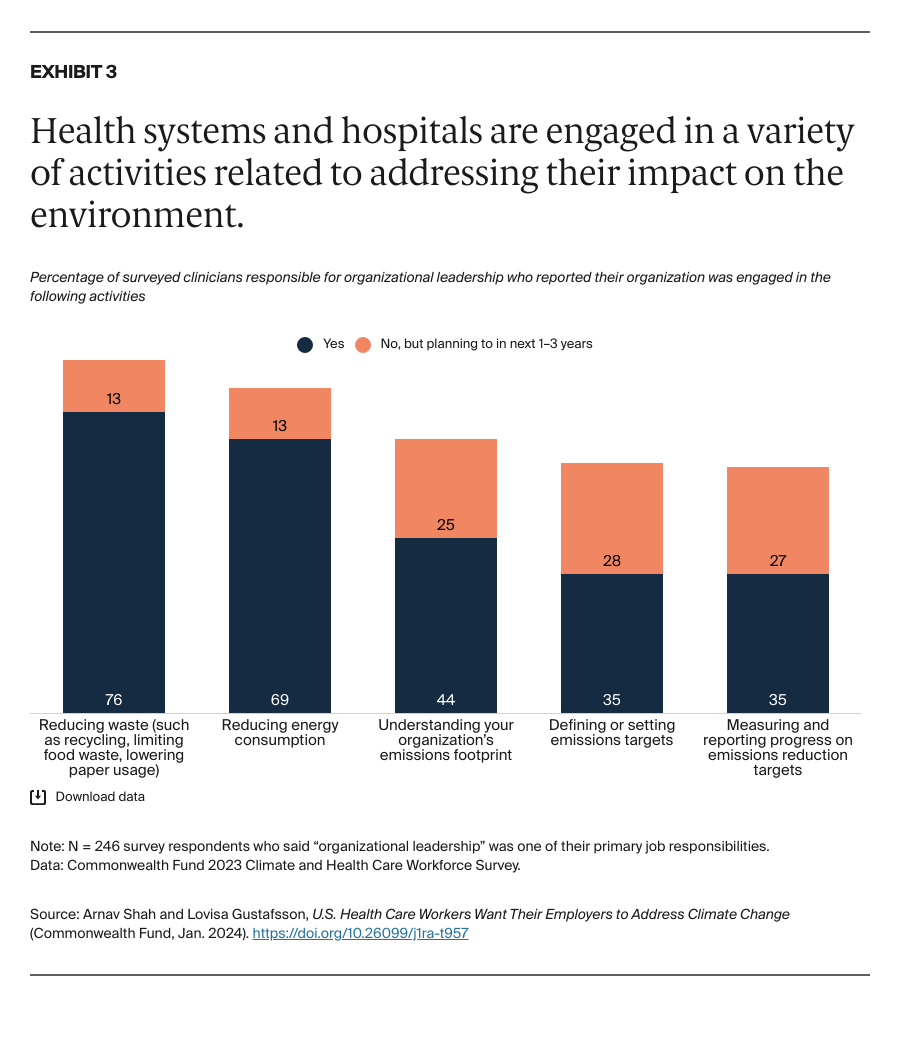
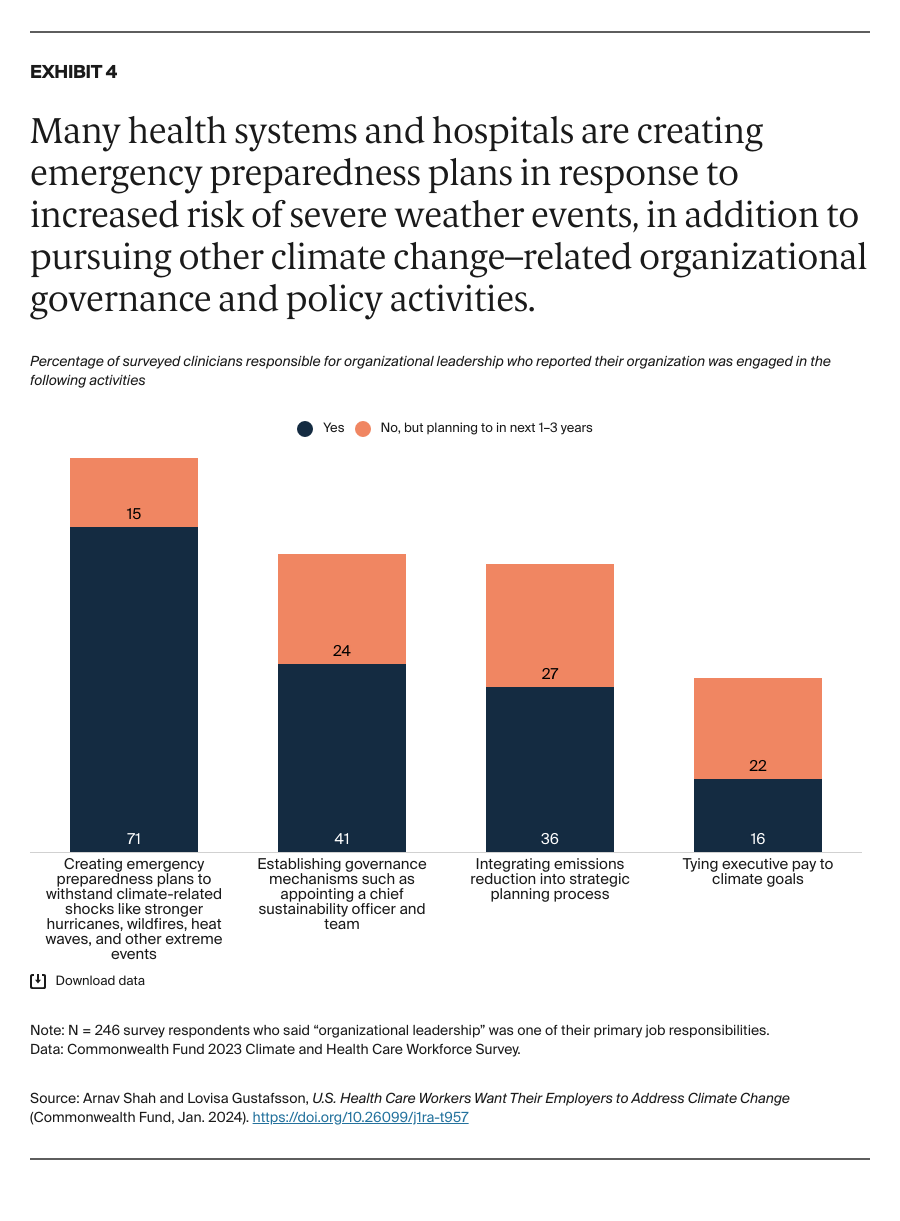
Within the United States, the health care sector is responsible for 8.5 percent of greenhouse gas emissions, largely from hospital care and from physician and clinical services.1 While a growing number of U.S. health care delivery organizations pledged to halve their emissions by 2030 and achieve net zero emissions by 2050, progress has been mixed. Many health systems have not made this pledge or taken meaningful steps toward decarbonization.2
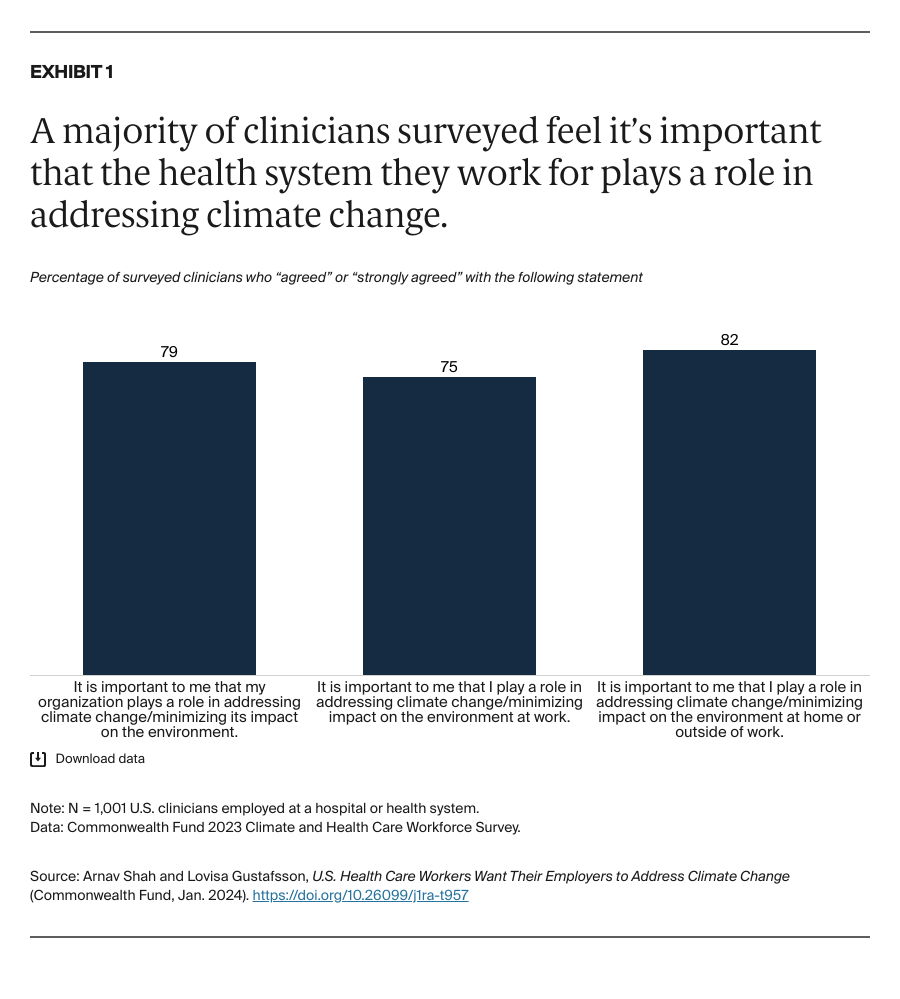
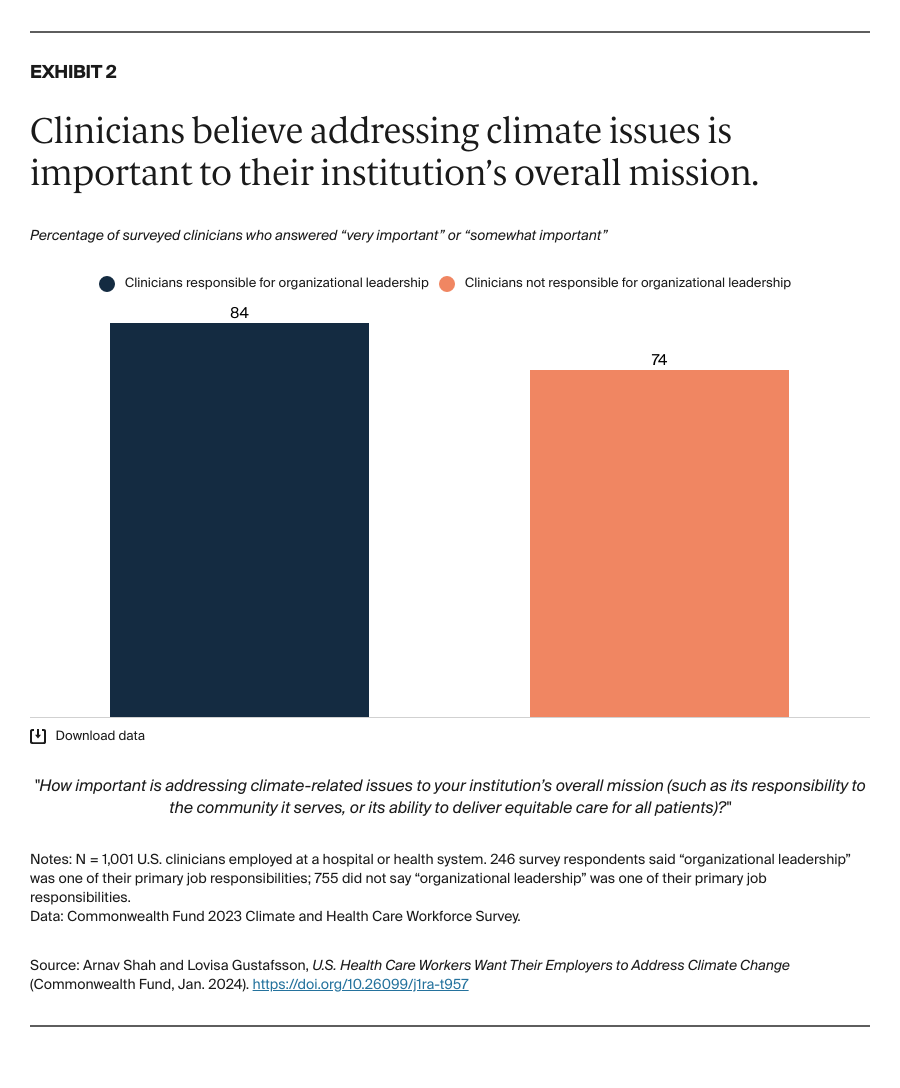
Effective sustainability and decarbonization efforts in health care require organizationwide buy-in to new innovations, policies, and procedures targeted at reducing waste and water consumption, adopting green building features, protecting facilities from extreme weather damage, converting to renewable energy, and other activities to advance a more sustainable health system.3 And buy-in from frontline health care workers — nurses, physicians assistants, nurse practitioners, primary care physicians, and specialists — is especially critical.
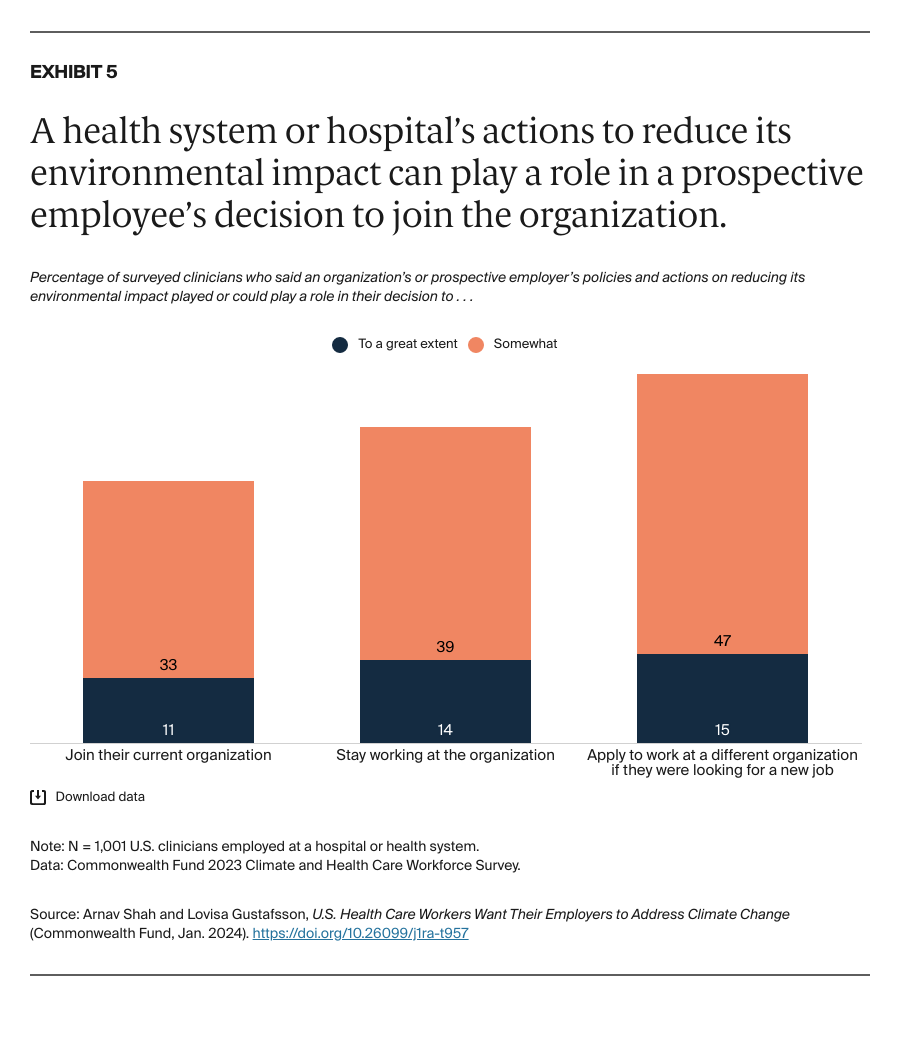
In this brief, we present findings from a national survey of 1,001 U.S. clinicians about their views of what health systems can do to address climate change. All those surveyed worked at a hospital or at a health system comprising more than one hospital; some had leadership responsibilities within their organization. (See “How We Conducted This Survey” for further details.) It is our hope that the findings could help motivate health care organizations to consider ways to decarbonize and reduce their environmental impact.