Policymakers Are Mobilizing to Address This Crisis
In response, policymakers at the federal and state level are considering behavioral health policy reforms. Legislative efforts are underway in Congress to advance bipartisan behavioral health policy solutions. The Biden administration has released national strategies for improving mental health and substance use disorder care, and has prioritized a range of critical behavioral health programs in the president’s 2023 budget. At the state level, policymakers are working to increase behavioral health access in community-based settings like schools, community health centers, and in the criminal justice system. State officials also have been actively implementing reforms to their existing crisis response systems in preparation for the launch of a new hotline callers can reach via the code 988 and are working to expand and diversify the behavioral health workforce.
Targeted Action Can Improve People’s Lives
Given the unique opportunity to advance evidence-based policymaking at the federal and state level, the Commonwealth Fund has committed to behavioral health policy research and activities in four areas:
1. Expanding Equitable Access to Behavioral Health Services
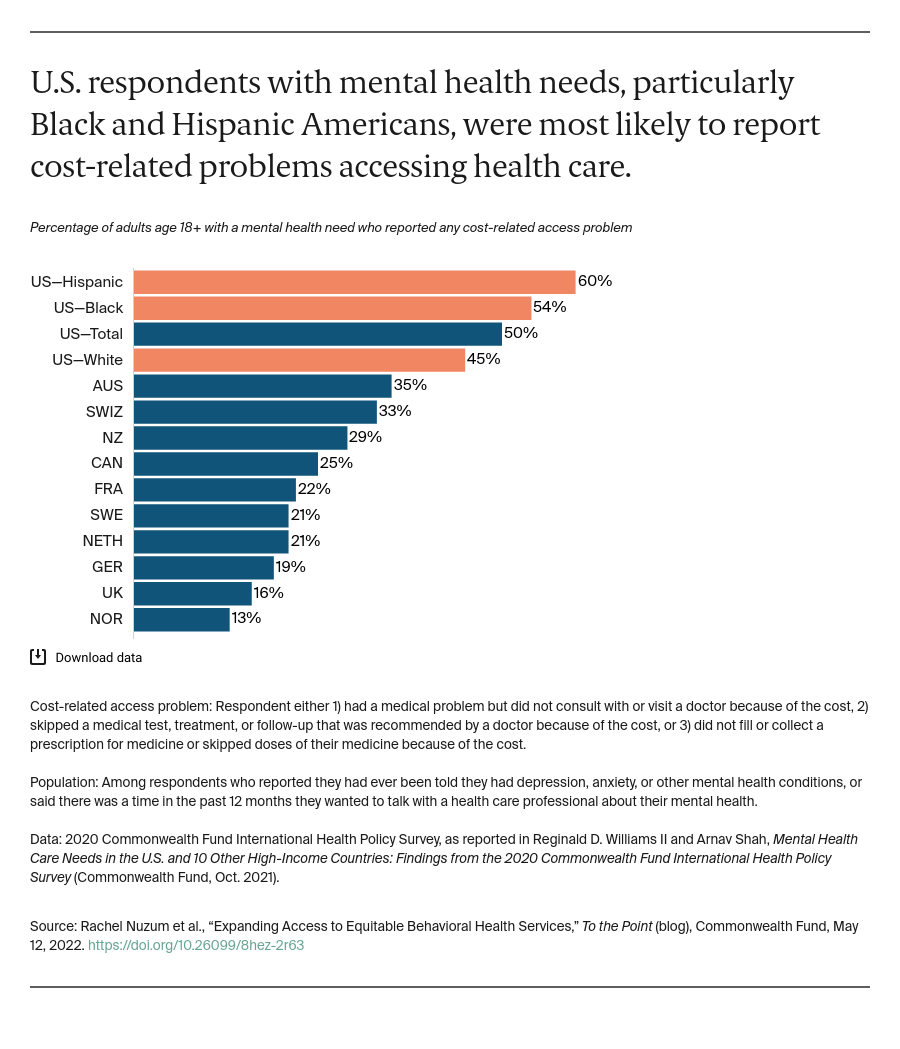
Efforts to expand access to behavioral health care have not closed gaps for Black people, Indigenous people, and other people of color. Racism, as well as structural inequities like lack of insurance coverage, income inequality, and an insufficiently diverse workforce contribute to the persistent gaps in access to behavioral health services.
Although telehealth flexibilities authorized early in the COVID-19 pandemic created new opportunities to access behavioral health providers, take-up varied greatly by race and ethnicity, geographic location, and payer source. The Fund will elevate evidence-based policies that address these racial disparities and advance access to health care services.
2. Integrating Primary Care and Behavioral Health
While U.S. primary care providers are making strides in treating the behavioral health needs of their patients, they are often working without necessary resources and supports. As many as 80 percent of people with behavioral health needs present in emergency departments and primary care settings; between 60 percent and 70 percent of these individuals leave without treatment for their conditions.
Because primary care offers a trusted and accessible source of care for many, expanding its capacity to address patients’ behavioral health needs has emerged as a key, cost-effective strategy for increasing access to behavioral health care. This approach, often referred to as “integration,” refers here to bringing together a range of providers and services within primary care settings to enable “whole person” care. The Fund will support the development of policy options that incentivize the delivery of integrated primary care and behavioral health services.
3. Strengthening and Diversifying the Behavioral Health Workforce
The behavioral health workforce cannot meet the current demand for services, nor is it equipped to provide the full range of care needed by individuals with behavioral health conditions. More than half of all rural counties report they do not have any behavioral health professionals and nearly three-quarters of all U.S. counties report serious shortages.
To address these gaps, paraprofessionals such as addiction counselors or community health workers are increasingly being integrated into the continuum of care. Sustaining and scaling these care models will require supporting payment and delivery models that include community-based providers. The Fund will advance the development of resources and policy options that support these models and incentivize the inclusion of community-based providers in the behavioral health workforce.
4. Leveraging Medicaid and Medicare
Medicaid is the largest payer of behavioral health services in the U.S. Yet, as a result of low reimbursement rates and an insufficient behavioral health workforce, many beneficiaries still lack timely access to care. Medicaid is especially important for children and adolescents, as the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit requires by statute that programs provide enrolled children and youth with all “medically necessary” care, including for a range of behavioral health needs.
Medicare beneficiaries also have significant mental health needs and face barriers in accessing care. Low-income seniors and others that qualify for both Medicare and Medicaid have particularly high behavioral health needs and report more challenges in accessing care when compared to either Medicaid or Medicare beneficiaries. The Fund will target opportunities to leverage Medicaid and Medicare programs to innovate behavioral health coverage, delivery, and payment models to reach those with disproportionately high needs.
The Next Steps Are Clear
Our behavioral health needs have never been greater, and the time is now for expanding equitable access to services. The problem is complex, but bipartisan commitments in Congress, leadership from the Biden administration, and the prioritization of the issue at the state level can pave the way for change. The Fund will help advance policy discussions and decisions to ensure that solutions address the disproportionate impact of the crisis on people of color, advance care and payment models that integrate behavioral health and primary care services, include community-based providers, and effectively leverage the power of our public programs.