This case study is the first in a series profiling how primary care clinics — federally qualified health centers, independent clinics, and clinics that are part of large health systems — are meeting the needs of patients with low incomes. An earlier series of case studies profiled care models serving frail elders and people with disabilities and/or multiple chronic conditions. We are now focusing on people who may not have such complex health care needs but are at risk of developing problems because they lack the resources to stay healthy. This series will profile clinics that exhibit some or all of the following attributes:
- medical home capabilities as a foundation
- multidisciplinary teams with community health workers
- integration of primary health care with public health, social services, and behavioral health
- using data to manage and improve patient care and clinic performance
- geographic empanelment, including appropriate risk stratification and targeting
- proactive patient and family engagement to address physical, social, and cultural barriers to care
- leveraging of digital tools to improve health
Stephen and Sandra Sheller 11th Street Family Health Services stands out as an exemplar of integrating physical and behavioral health services.
Background
Stephen and Sandra Sheller 11th Street Family Health Services of Drexel University — a federally qualified health center in North Philadelphia operated in partnership with the Family Practice & Counseling Network — sits in a neighborhood in transition. Four public housing developments and a scruffy bodega surround the center, but blocks away are new bars, restaurants, a gin distillery, and rehabbed rowhouses — all signs of the gentrification taking place in pockets across a city that still ranks as the poorest of America’s major metro areas.1
The health center grew out of an effort in the late 1990s to serve the neighborhood’s many public housing residents, whose high rates of diabetes, cardiovascular disease, and other chronic conditions were compounded by poor access to primary care. Residents felt like they lived in a world apart, contending with decades-old public housing with antiquated plumbing that caused raw sewage to back up in sinks and bathtubs, electrical systems that frequently left them in the dark, and drug dealers operating in the maze of courtyards.
You can easily look at health stats and see what is happening but you need to connect with the people. You can’t walk into a community and say, “I know what your problem is.”
Acting in partnership with the Philadelphia Housing Authority, Patricia Gerrity, R.N., Ph.D., then associate dean for community programs at the Medical College of Philadelphia/Hahnemann University, began knocking on doors and attending public housing residents’ council meetings. It was slow going. “The residents were really not interested. They were tired of being assessed and surveyed by people like us from universities who only stuck around until their research ended,” she says.
Gerrity and a few other nurses spent years earning people’s trust, mainly by showing up and delivering practical solutions. At community members’ behest, they began visiting seniors in their homes to help them manage chronic conditions. They lobbied the city to place a stop sign on a dangerous intersection and created an emergency food pantry for people whose grocery money ran out at the end of the month. When they heard that ambulances struggled to find people in the sprawling public housing complexes — one woman’s son bled to death in her arms — they offered free training in CPR and other lifesaving techniques.
By 1998, the nurses had opened a free clinic in an unused public housing unit. After a few years, they convened a community planning session to discuss how to build on their efforts; the session lasted 16 hours and drew people from the public housing developments, local businesses, schools, churches, and the public health department. A clear message emerged: “Community members wanted some place where they could be healthy, not just a place to go when they were sick,” says Roberta Waite, Ed.D., R.N., 11th Street’s executive director.
The nurses eventually secured funding from the Health Resources and Services Administration and the Philadelphia Housing Authority to build a full-scale health center. The 17,000-square-foot space opened in 2002 on ground cleared when the city tore down the old public housing complexes and built condo-style units.
Since then, 11th Street Family Health Services has been jointly operated by Drexel University’s College of Nursing and Health Professions and the Family Practice and Counseling Network, a nonprofit health and behavioral services provider that holds the federally qualified health center (FQHC) license and manages the finances.2
In this case study, we describe how 11th Street’s leaders, staff, and patients have hewn to the founding vision of a center focused on health, not sickness.

Building a Center for Health
To promote health in its neighborhood, 11th Street’s founders looked to international models, including the U.K.’s Peckham Experiment, a 1930s plan to improve residents’ health in a working-class South London neighborhood by offering nutritious food, opportunities to exercise and socialize, a library, day care, and other supports. They studied healthy living centers formed as part of a 1990s initiative to reduce health disparities between low- and high-income Britons. In 2003, Gerrity visited a healthy living center catering to Bangladeshi immigrants, with a kitchen and event space, and another where art therapists helped people struggling with alcohol addiction. These models’ expansive view of health as more than just medical treatment and their focus on building strong communities became part of 11th Street’s approach.

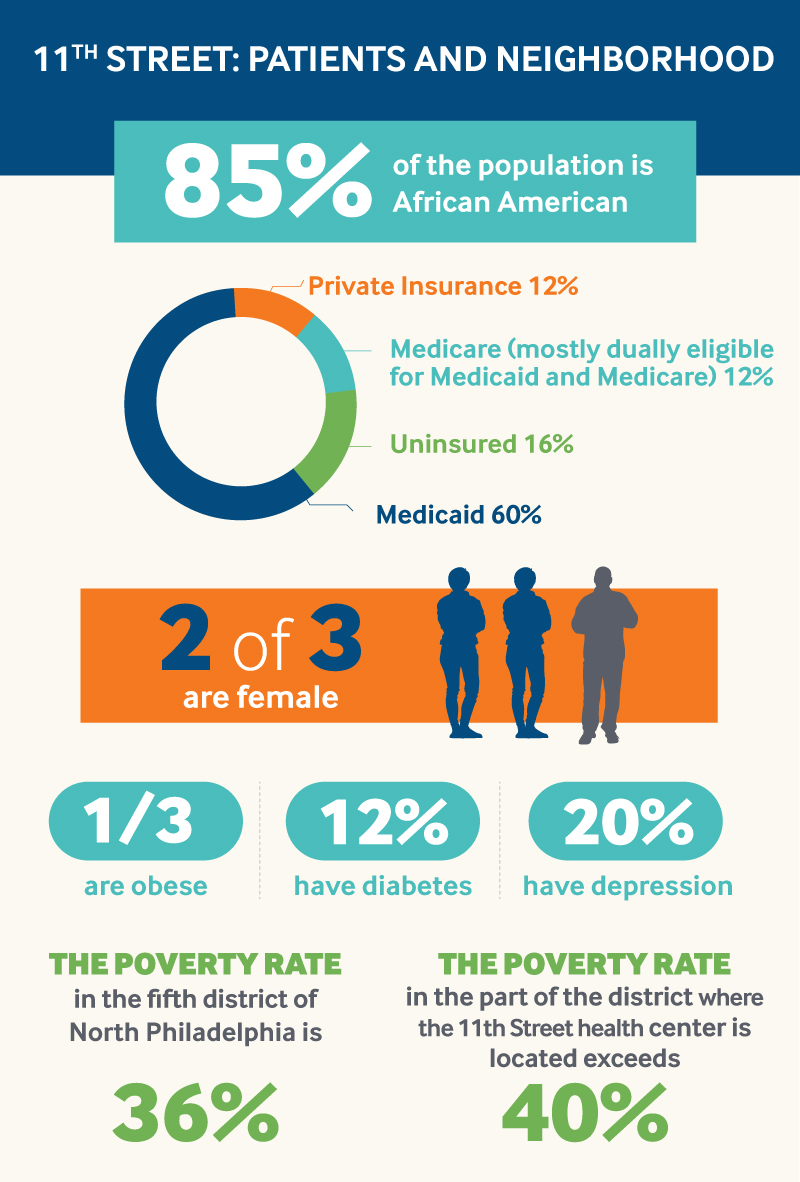
Most of 11th Street’s 6,000 patients live in local public housing, but some travel to the health center from other parts of the city or nearby suburbs, after having moved out or been priced out of the neighborhood. Most are African American women covered by Medicaid; significant numbers have chronic conditions including hypertension (appearing even among young adults and children), heart disease, diabetes, depression, and chronic pain. About 15 patients serve on the Community Advisory Committee and play an active role in shaping services and building relationships with local schools, churches, and nonprofits.
The difference from a traditional primary care clinic is noticeable in 11th Street’s lobby, which brims with activity: people hurrying to a yoga class or a support group, or picking up boxes of fresh fruit and vegetables from Lancaster County farms. Elsewhere, men and women join drum circles, work out at the gym, or take mindfulness training or creative arts therapy. These are some of the ways the center has sought to engage people and help them build health and resiliency. Many of these services were added in response to evidence that patients had experienced traumatic events and were coping with both mental and physical health problems. Initially, 11th Street’s leaders used grants to pay for these new services. Some were eventually added to the FQHC operating budget as leaders gathered evidence of their effectiveness, and a handful have begun to be reimbursed by payers, as described below.

A Medical Home and Beyond
11th Street is certified by the National Committee for Quality Assurance as a Level III Patient-Centered Medical Home. Primary care teams include nurse practitioners, registered nurses, medical assistants, social workers, behavioral health consultants, and a nutritionist. There are no staff physicians, making it one of about 250 nurse-led FQHCs among nearly 1,400 centers nationwide.3 It has traditional behavioral health services as well as creative arts therapies, a dental clinic, laboratory, and a private pharmacy, which makes deliveries throughout the city. It also offers same-day and after-hours appointments, free van rides to appointments, and a nurse triage hotline.
Every six months, patients are asked to answer questions about their mood and childhood experiences. If the responses suggest problems, patients are asked to complete the full PHQ-9 survey, which asks about their mood, sleep habits, appetite, and day-to-day functioning, and the adverse childhood experiences (ACE) survey, which covers instances of violence or neglect. In addition, an AmeriCorps volunteer greets patients in the lobby and asks them to complete an “interest form” indicating their health and social needs; a staff member follows up to offer services.
Patients with chronic medical conditions receive comprehensive assessments, including home visits. Care teams follow shared plans to manage their conditions.
Addressing Basic Needs
Well before research on the “social determinants of health” had become mainstream, 11th Street’s leaders recognized that many people get sick because they don’t have the basic resources to stay healthy.4 Nearly all (about 90%) of patients receive help for things other than medical problems: working with a social worker to enroll in health insurance or other benefits, finding educational or job training programs, or creating a budget. Many receive free legal services on issues like eviction, unsafe housing, and domestic abuse.
Given that produce at the local grocery store is too expensive for many residents, 11th Street has partnered with the Farm to Families Initiative, which provides weekly deliveries of subsidized fruits and vegetables to patients eligible for or enrolled in the Supplemental Nutrition Assistance Program (SNAP). Over 300 families participate. Jennifer Warshaw, M.S., M.P.H., R.D.N., director of nutrition education services, offers recipes, cooking classes, and food demonstrations in the teaching kitchen, as well as counseling and mindfulness training to patients wishing to change their eating habits. Acknowledging that “no one wants to see a nutritionist,” she’s tried to keep things fun by holding Battle of the Chefs–style competitions, or offering “A Taste of African Heritage,” which teaches people how to use the traditional foods of the African diaspora.
If it wasn’t for this health center, I would never have known about ACEs. I will always remember Patty [Gerrity’s] words: “When you see a child acting out, the question isn’t, ‘What’s wrong with that child?’ It is, ‘What has happened to that child? What has happened to that parent? What has happened to that parent’s parent?’”
Identifying and Responding to Trauma
Over the years, 11th Street’s clinicians heard stories from patients about domestic violence, rape, or other traumatic experiences, or noticed troubling signs of these experiences. Gerrity recalls hearing from a mother whose child had suddenly begun wetting the bed after he saw her stab her boyfriend and from a grandmother whose grandson had tried to rob her in order to buy drugs.
Stories of traumatic experiences also surfaced during a women’s diabetes management group. “The educator was great, the reading level of the materials was appropriate, but we weren’t getting results,” Gerrity said. When a behavioral health specialist began meeting with the women, she discovered that many had undiagnosed depression — and a shared history of childhood and/or ongoing abuse. “Each one thought they were the only ones,” Gerrity said.5
The Effects of Trauma in Families and Neighborhoods
Since the original ACE study, scientists have identified some of the ways traumatic experiences can have long-term impacts on brain development, physiology, and behavior. These include changes in the way we perceive pleasure and rewards, changes to the brain and hormonal systems that react to perceived threats, and even genetic changes that can affect the immune system.6 People who experience prolonged or repeated adversity may experience “toxic stress” that can take a toll on human development and lead to long-term health problems. Some who’ve experienced trauma turn to coping behaviors, including unhealthy eating and substance abuse.7
Researchers have begun to look at how trauma not just within families but in schools, streets, and neighborhoods can affect health. In 2012, 11th Street Family Health Services and members of the Philadelphia ACEs Taskforce used an expanded version of the ACE survey that asked adults whether as children they had: witnessed violence other than a mother being abused, experienced race-based discrimination, felt unsafe in their neighborhood, been bullied, or had been in foster care.
Among 1,784 Philadelphia residents, two of five (40.5%) had witnessed violence while growing up, such as seeing or hearing someone being beaten, stabbed, or shot. More than a quarter (27%) reported having felt unsafe in their neighborhoods, while more than a third (34.5%) said they had experienced discrimination based on their race or ethnicity.8
To delve into how racism affects their work, 11th Street’s staff members take part in sessions about the impact of structural racism and discrimination. “We hone in on how race affects what we do and how we interact,” says Waite. The health center is now launching a series of educational sessions on the intersections of trauma, racism, and health.
To investigate how common such experiences were, Waite and Gerrity screened 801 patients (647 women, mostly African American; 154 men, mostly African American) using the ACE survey. This screening tool was developed in the late 1990s by a Kaiser Permanente physician who discovered that many of his obese patients had a shared history of childhood sexual abuse; he theorized that overeating and other unhealthy behaviors might be coping strategies. The survey asks adults whether as children they had experienced physical, emotional, or sexual abuse; neglect; lived with someone who was abused, mentally ill, incarcerated, or struggled with substance abuse; or had divorced or separated parents.
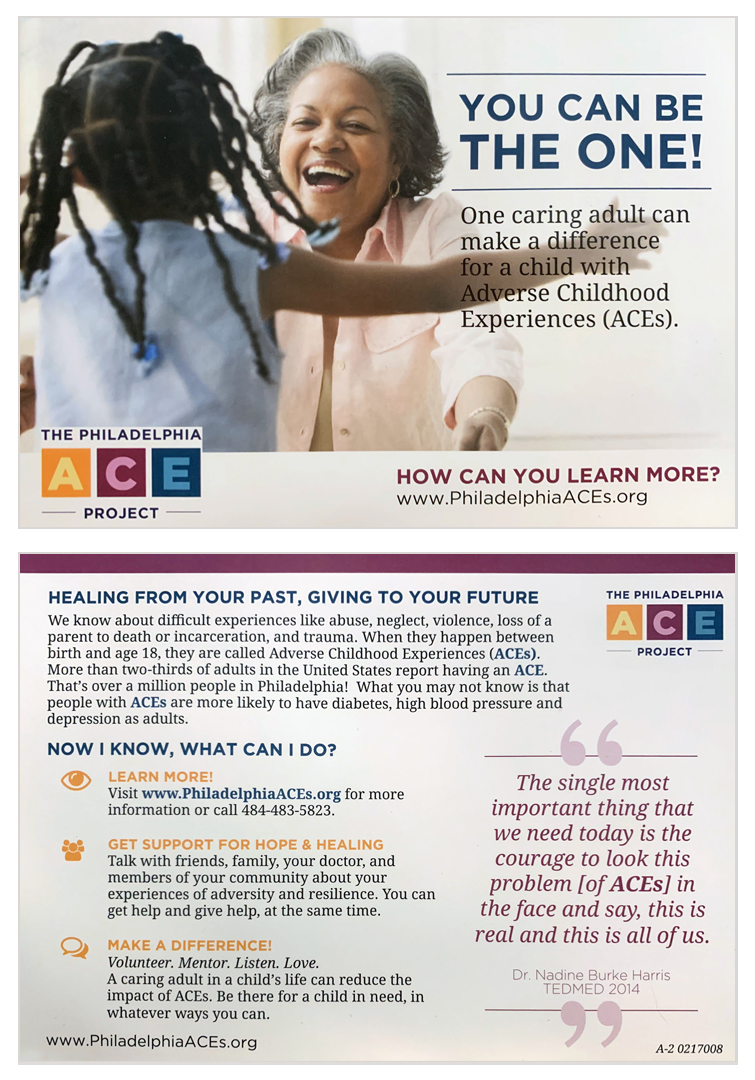
The results of 11th Street’s 2009–10 study — one of the first to explore childhood adversity among low-income, minority patients in primary care — were startling. While 64 percent of the original Kaiser respondents (mainly white and middle-class) reported at least one type of adverse childhood experience, nearly all (94%) of 11th Street’s patients did. While 12.5 percent of Kaiser respondents reported four ACEs, nearly half (49%) of 11th Street’s patients did. Confirming prior studies, 11th Street researchers found that patients who had experienced adversity as children were more likely to be sick, particularly with diabetes and/or depression. There was a cumulative effect: the more types of adverse experiences they had lived through, the more likely they were to be sick.9 They were galvanized by the findings: “Having the data gave us an obligation to do something,” says Gerrity.
Engaging Community Residents in Conversations About Violence, Abuse, and Trauma
11th Street was an early adopter of “trauma informed care,” which focuses on raising awareness of trauma and its effects on health and creating safe clinical environments that are less likely to trigger traumatized patients. Most health care organizations that have adopted trauma-informed approaches screen patients and educate them about the link between trauma and unhealthy behavior and poor health outcomes. They also may enhance access to treatment by streamlining referral pathways to specialty care or embedding behavioral health providers in primary care settings. 11th Street has gone a step further by adding creative arts therapies and other counseling services that target the negative effects of trauma, including stress and distrust.10
In September 2018, 11th Street became the first primary care provider to become a Sanctuary center, a model adopted by mental health providers, juvenile justice programs, homeless shelters, and domestic violence programs to help traumatized patients.
11th Street recognizes that patients who are racial minorities are less likely than others to ask for help when they experience mental health problems and that some (particularly children) may come to regard traumatic events such as gun violence and crime as normal. To address this, 11th Street’s leaders launched a campaign to educate community members.11 In 2012, Gerrity and members of the Community Advisory Committee took an Institute for Healthcare Improvement course on how to lead change and got advice from a University of Pennsylvania researcher who studies what makes ideas spread. They used a postcard campaign to educate people about ACEs — encouraging them to speak up if they or a loved one has been affected by violence, abuse, or neglect and let them know healing is possible.
Detecting Problems Early
The health center’s leaders have sought to prevent traumatizing childhood experiences by breaking generational cycles of violence or abuse and promoting strong families. They ask all pregnant women to take the ACE survey to detect instances of childhood trauma, and connect women who’ve experienced trauma to therapy or other supports. They also refer first-time mothers to the Nurse Family Partnership, a program in which nurses visit mothers at home during their pregnancies and their children’s first two years.
An 11th Street social worker, known as a family, child, and support coordinator, meets with families when women first become pregnant through their children’s teenage years to assess family relationships, promote positive parenting skills, detect emotional and developmental problems, and offer referrals to early intervention services. If fathers are present at visits, the coordinator will emphasize the important role they play; if not, she will ask about their involvement and encourage them to attend future visits. This service has reduced the number of children being referred to medical specialists for conditions like bedwetting that can have roots in emotional problems.12
The health center has gradually rolled out ACE screening to all adults receiving primary care services as it has added sufficient resources to respond to identified problems.
Creating a Safe, Welcoming Environment
As part of its efforts to help patients, 11th Street’s leaders have encouraged staff members to care for themselves. All are offered mindfulness training to help them cope with the stress of working in a busy environment and being exposed to stories of trauma and so they can model mindful practices for patients. Lekisha Parker, C.M.A., lead medical assistant, uses mindfulness techniques with patients who feel anxious about their medical visits.
In treating our patients, what matters is not so much what we do but how we do it.
Offering a Range of Therapeutic Approaches
Over the past several years, 11th Street has added creative arts therapies as well as yoga, meditation, and mindfulness training to complement traditional counseling options.
Anyone can drop in to take a class or try creative arts therapy. “We had to reconceptualize the definition of a patient,” says Kathleen Metzker, M.P.H., director of integrative health and mind–body services. “Someone can enter the center through any entry point; there is no wrong door.”
These nontraditional therapies have encouraged more patients to seek treatment. Some have been willing to try them because they are more convenient, while others see them as less stigmatizing or intimidating than traditional therapy. “We’ve found that some patients need different approaches in order to make sense of their trauma; it’s important to give them choices,” says Gerrity. Some patients start with creative arts therapy or meditation and eventually try traditional counseling; these patients tend to make the most progress.

From the beginning, Gerrity emphasized these new therapies were core parts of their clinical approach and not “alternative” services. The mind–body teacher, for example, uses breathing exercises, guided visualizations, and other methods to help people pay attention to their sensations and emotions without interpretation. Such approaches have been shown to reduce anxiety and promote calm responses — helping to counter the instinct toward “flight or fight” that may be triggered by stressful experiences.
Music therapists have offered “Power Over Pain” sessions, which involve singing elongated vowels, humming, and deep breathing, as well as group singing and vocal improvisations to help people cope with chronic pain. Lindsay Edwards, M.A., L.P.C., director of creative arts therapies, offers a dance/movement therapy class to support grandparents raising grandchildren. “We notice how we can feel more in control moving at a slower pace, and we notice that we’re not alone in tackling similar hardships,” she says.
Patients who need medication management (e.g., for post-traumatic stress disorder or major depression) are referred to Sarah Thornburg, M.S.N., C.R.N.P., a psychiatric nurse practitioner. Thornburg also provides medication-assisted treatment to patients with opioid-use disorder.
Integrating Medical and Dental Care
Many people avoid dentists because they worry about the costs or pain of treatment; those who’ve experienced trauma may fear an experience of lying prone and being unable to speak. For all, the longer they wait, the harder it feels to go.
To encourage more patients to receive regular dental services, 11th Street launched a medical–dental integration program in 2016. Every day, a coordinator runs a report to identify patients coming for a medical visit who haven’t seen a dentist in the past year. After their visit, primary care clinicians invite these patients to undergo a brief oral health screening to look for signs of periodontal disease, decay, or other problems. While this service is offered to all, the health center has focused on those at greatest risk: children, pregnant women, and people with diabetes or hypertension.
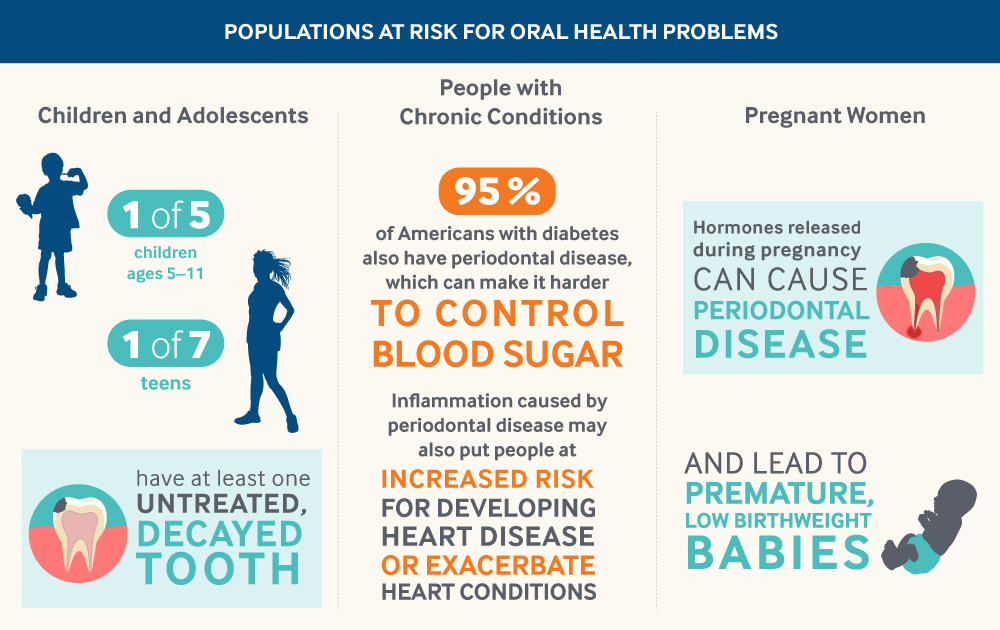
Moving a dental office to the primary care suite and tag-teaming visits “increases the chances people will be willing to receive dental services,” says Dana Robinson, R.D.H., P.H.D.H.P., 11th Street’s public health dental hygiene practitioner. “Some of our patients haven’t seen a dentist in 10 or 15 years, so we don’t tend to do cleanings right away. We do an assessment and take x-rays. I tell them it’s just baby steps.” Robinson also invites Drexel music therapy students to provide music during visits to help with anxiety. The health center has seen a 25 percent increase in new dental patients this year, which it attributes to the greater comfort and ease of access.
Assessing Impact
11th Street performs as well as or better than the national average among FQHCs on nearly all measures of disease prevention and control reported in the Uniform Data Set. In particular, it does better than the national average among FQHCs in documenting patients’ body mass index and offering plans to help them achieve healthy weight (83% of patients vs. 64% nationally). More 11th Street patients have achieved diabetes control (75% of diabetic patients have an HbA1c less than 9% vs. 66% nationally). It does less well in controlling blood pressure among hypertensive patients (56% of patients vs. 63% nationally).
It has struggled to engage patients in certain screenings; in 2017 just 31 percent of children had received recommended vaccinations (Rotovirus and influenza) by age 2, compared with 40 percent nationally.13 Strategic initiatives to close this gap, including better tracking and follow-up, led to a 10 percent increase in immunization rates and recognition from the Philadelphia Department of Public Health.
Additional evidence suggests that 11th Street’s focus on developing strong families through prevention and early intervention has paid off. The health center has reduced preterm births to 2.5 percent among African American women, compared with nearly 16 percent across the city.14
To measure the impact of their efforts, 11th Street’s leaders mainly use the Short Form Health Survey, which focuses on quality of life rather than clinical benchmarks. It asks people to report on their physical and emotional well-being using plain language and say whether they’re able to complete day-to-day tasks. “We want to know whether people’s lives are changing,” says Gerrity.
11th Street has used this survey to assess the effects of the mind–body interventions as well as creative arts therapies. In one study, patients who participated in four mindfulness sessions experienced decreased anxiety and improvements on measures of mental and physical functioning, social functioning, and vitality.15 In another, patients with chronic pain who participated in eight music therapy sessions reported somewhat less pain and were much more likely to say they felt able to work, complete chores, and socialize than a control group. They also reported greater feelings of motivation, empowerment, and sense of belonging.16

Lessons
11th Street Family Health Services offers lessons for other primary care clinicians working to promote health and resiliency for low-income patients.
Promoting Health Requires R&D
11th Street has benefitted from having seasoned leaders who are both practical and research-driven; they’ve listened to what people need, responded in creative ways, and studied the results. “My job essentially was to continue to learn about the community, to look at those who come for care, those who don’t, try to figure out what they need and what’s the best practice that could address those needs — whether insurance paid for it or not — and then try to do it,” says Gerrity. “And then see if it works.”
Because 11th Street’s nurse leaders do not control the operating budget (Family and Practice Counseling Network, the FQHC licensee, does), they’ve relied on financial support from Drexel University and private philanthropies to pilot new services that are not reimbursed. Their willingness to experiment has begun to pay off; in 2018, a policy change enabled the health center to begin billing Medicaid for the services of licensed professional counselors, including some of the creative arts therapists. Evidence of the effectiveness of the child and family support coordinator, who had previously been paid through grants, convinced the Family and Practice Counseling Network to pay for some of her salary. “We’re an incubator for ideas,” says Waite.
Positive Approaches Are Key to Engagement
11th Street clinicians have been able to earn their patients’ trust and engage them in treatment because they’ve focused on health, not sickness. This positive approach is evident in the health center’s creative efforts to promote healthy development, including dance therapy sessions that encourage teen girls to develop positive body images. It’s also part of its approach to therapy. “We’re really quick to say, ‘This is what’s wrong with me,’” says Metzker. “We try to say ‘What is right with you, what’s working?’ When we bolster that we can get to problem-solving and let people experience the best parts of themselves.”
Like many community health centers, 11th Street serves predominantly women.17 To engage more men in care, in 2016 the health center sought and received funding from AstraZeneca HealthCare Foundation to engage young men at risk for cardiovascular disease. The initiative aims to help increase their understanding of nutrition and cardiovascular disease, in part through a peer learning group. The health center is also launching a music therapy group for adolescent males and hoping to recruit more male clinicians.18
Attend to the Role of Trauma in Poor Health
While focusing on positive approaches, 11th Street’s leaders have been clear-eyed about the damage inflicted by patients’ traumatic experiences. They’ve emphasized the need to shed light on problems and continue to offer “ACEs 101” training for members of the Community Advisory Committee, who give presentations in their churches, schools, and workplaces. They also acknowledge that the healing process can be long and messy, and have therefore put no parameters or requirements on patients receiving services.
11th Street’s Future in a Changing Neighborhood
The model of inclusiveness extends to new residents of the rapidly gentrifying area. Members of the Community Advisory Committee recently launched an effort to serve as patient ambassadors to make sure all neighborhood residents know about the health center’s many services. “Our community is changing. And we want to get the word out that 11th Street is not exclusively for people with low income. It’s for anyone,” says Jacqui Williams, a longtime member of the Community Advisory Committee. “This center is a beacon here in this community.”
Acknowledgments
11th Street Family Health Services: Senetta Boyd, M.S.W., Tawanna Cooper, R.N., Lindsay Edwards, M.A., L.P.C., Madeline Frank, Patricia Gerrity, R.N., Ph.D., Diana Hartley-Kim, M.S.W., Paula Larson, M.S.N., M.P.H., Kathleen Metzker, M.P.H., Diane Monroe, Lekisha Parker, C.M.A., Dana Robinson, R.D.H., P.H.D.H.P., Lidyvez Sawyer, M.P.H., Yael Tacher, Sarah Thornburg, M.S.N., C.R.N.P., Roberta Waite, Ed.D., R.N., Jennifer Warshaw, M.S., M.P.H., R.D.N., and Jacqui Williams. Commonwealth Fund: Melinda Abrams, M.S., and Yaphet Getachew.
Commonwealth Fund case studies examine health care organizations that have achieved high performance in a particular area, have undertaken promising innovations, or exemplify attributes that can foster high performance. It is hoped that other institutions will be able to draw lessons from these cases to inform their own efforts to become high performers. Please note that descriptions of products and services are based on publicly available information or data provided by the featured case study institution(s) and should not be construed as endorsement by the Commonwealth Fund.


