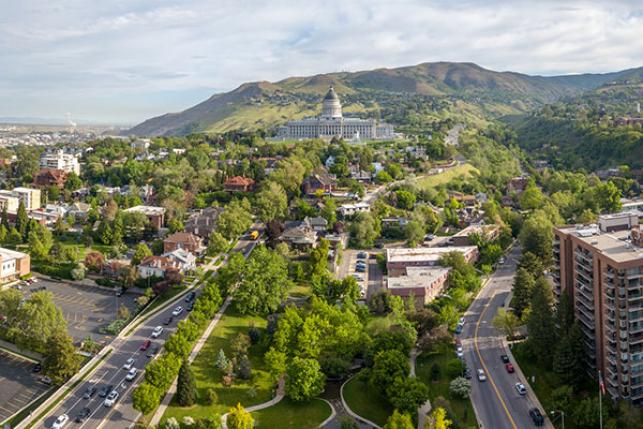
One Step Forward, Two Steps Back: Utah’s Medicaid Expansion
A provision in Utah’s Medicaid waiver that allows the state to close enrollment at any time has significant implications for health coverage. An enrollment cap in Utah’s Medicaid program could discourage people from changing jobs or adding work hours, as they might have trouble regaining coverage.







